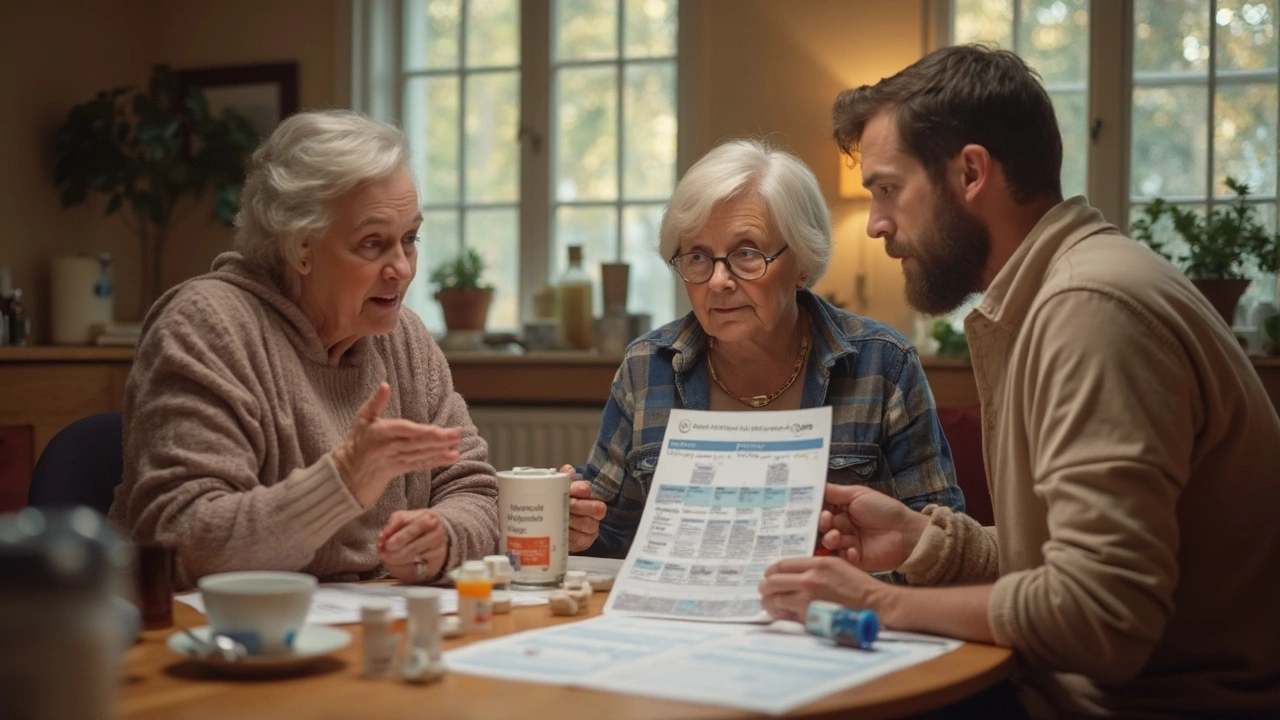
Furosemide’s been the classic go-to when doctors want to clear out extra fluid fast, but it’s definitely not the only game in town anymore. By 2025, we’ve got more choices—some with fewer side effects, others that fit better for certain health issues. People who deal with high blood pressure or swollen ankles know how tough it is when their meds cause other problems like low potassium or constant bathroom trips.
So, why stick to the same old routine if there are fresh alternatives? Modern diuretics—not just furosemide—each have their own quirks: some protect your potassium, some are easier on your kidneys, some play well with combo therapies. Knowing your options gives you and your doctor more ways to dial in the right balance and avoid those annoying side effects that hijack your day.
Let’s break down what's new, what actually works, and what to watch out for—so you can have smarter talks at your next appointment.
- Why Look Beyond Furosemide?
- Amiloride
- Chlorthalidone
- Hydrochlorothiazide
- Spironolactone
- Side-by-Side: Choosing the Right Alternative
Why Look Beyond Furosemide?
For ages, furosemide alternatives barely got a look because furosemide worked fast and was pretty cheap. But as more people use it long-term for things like heart failure, kidney problems, or stubborn swelling, the cracks have started to show. Some folks end up with super low potassium, muscle cramps, or even dehydration—you know, the kind of stuff that ends in a trip to the ER.
The catch with furosemide? It hits hard but sometimes a bit too hard. It can flush out crucial minerals like potassium and magnesium, which are honestly just as important as clearing away water. This can cause side effects like weakness, irregular heartbeat, and major fatigue. If you’re trading off being less swollen for feeling like you just got hit by a truck, then something’s gotta give.
Another thing: not everyone’s body reacts to furosemide the same way. Over time, a lot of patients see the effect drop off—a phenomenon called “diuretic resistance.” Your kidneys just stop caring, and the water weight comes right back. In 2025, doctors want to avoid the back-and-forth cycle where you have to change doses all the time or combine drugs that don’t play nice together.
If you’ve seen your doctor switch you from one pill to another, you’re not alone. Here’s a quick table showing common issues with furosemide that lead people to hunt for something else:
| Problem with Furosemide | Impact |
|---|---|
| Low potassium | Muscle cramps, weakness |
| Dehydration | Dizziness, dry mouth |
| Frequent urination | Interrupted daily life |
| Less effective over time | Fluid returns, need higher dose |
The bottom line? Exploring new diuretics 2025 isn’t just about swapping one pill for another. It’s about finding a treatment that actually fits your life, not just your lab numbers. There’s no one-size-fits-all, so understanding the latest choices sets you up for a better daily routine and fewer surprises.
Amiloride
Looking for a furosemide alternative that’s a little gentler on your body? Amiloride is worth a closer look, especially if you’re worried about losing too much potassium. Unlike furosemide, which can zap potassium straight out of your system, amiloride is a potassium-sparing diuretic. That basically means it helps kick out extra salt and water but hangs onto potassium. This makes it a favorite for folks prone to muscle cramps or arrhythmias from low potassium.
Doctors often use amiloride for fluid retention and high blood pressure, sometimes on its own but more commonly with another diuretic, like hydrochlorothiazide, to get the best of both worlds. You’ll see it pop up in combination pills, shrinking down your daily pill count. And if you’re looking for something for long-term use—say, for chronic swelling from heart failure or high blood pressure—amiloride holds up pretty well in the long run.
Pros
- Less likely to push potassium dangerously high compared to other potassium-sparing diuretics like spironolactone.
- Works well as part of combo therapy, like with thiazide diuretics, so you get better blood pressure or swelling control without the rollercoaster of side effects.
- Easy to take once a day for long-term management of edema and hypertension.
Cons
- Not as strong by itself—if you need big-time fluid removal like furosemide gives, amiloride alone probably isn’t enough.
- Combining it with other diuretics means extra monitoring for things like sodium levels (watch out for low sodium).
- It’s usually not the first pick when you’ve got severe kidney problems since it’s filtered by the kidneys.
One thing to keep in mind: If you’re getting frequent bloodwork, like most folks on diuretics do, amiloride usually makes it easier to keep potassium in the sweet zone. And since it won’t cause as much hormonal trouble as some others (looking at you, spironolactone), you’re less likely to run into weird side effects like tenderness or changes in libido.
Here’s a quick way to see how amiloride stacks up for key concerns:
| Feature | Furosemide | Amiloride |
|---|---|---|
| Potassium Loss | High risk | Low risk |
| Strength (Edema Control) | High | Mild to moderate |
| Best For | Severe edema | Mild edema, combo therapy |
| Long-term Use | Yes, with monitoring | Yes, good for chronic needs |
Chlorthalidone
If you want a furosemide alternative that’s solid for blood pressure and works long, chlorthalidone is worth a look. This thiazide-like diuretic has been used for decades and has outlasted a lot of trends in the pharmacy world. What people usually like is how it keeps blood pressure steady all day—better than hydrochlorothiazide in lots of cases.
Doctors often turn to chlorthalidone if you’ve got high blood pressure (hypertension) and mild swelling, not extreme fluid overload. It’s a favorite in guidelines for treating hypertension because one pill can control blood pressure for 24 hours thanks to its slow, steady effect. Chlorthalidone is even included in the big ALLHAT trial that showed it cuts the risk of heart attacks and strokes as well as fancier, newer drugs. Some folks find their swelling goes down without those dramatic ups and downs furosemide sometimes causes.
Pros
- Long-lasting—one pill can work all day, helping you avoid that afternoon surge in blood pressure.
- Proven to lower heart attack and stroke risk according to big, long-term studies.
- Lower risk of sudden drops in blood pressure compared to loop diuretics like furosemide.
- Effective for salt-sensitive hypertension and mild fluid retention.
Cons
- Can lower potassium, so you might need regular blood tests or a supplement.
- Not as strong as furosemide for clearing major fluid overload (like in severe heart failure).
- May raise blood sugar and uric acid levels, so people with diabetes or gout should keep watch.
- Frequent urination might stick around, especially in the first few weeks.
Need the numbers? Here’s how chlorthalidone stacks up to furosemide and another common option for lowering blood pressure over 24 hours:
| Drug | Duration (hours) | Strongest Use | Low Potassium Risk |
|---|---|---|---|
| Chlorthalidone | 24-72 | Hypertension | Moderate |
| Furosemide | 6-8 | Severe Edema | A lot |
| Hydrochlorothiazide | 6-12 | Hypertension | Moderate |
If you’re talking to your doctor about switching off furosemide, chlorthalidone is a strong contender for daily control—just stay on top of those labs to catch any potassium drops or changes in sugar.

Hydrochlorothiazide
If you’ve ever taken a medicine for high blood pressure or mild edema, there’s a good chance you’ve come across Hydrochlorothiazide. This is a thiazide diuretic, totally different from furosemide, and it works by helping your kidneys get rid of extra salt and water. It’s especially common in combo tablets with blood pressure medications—makes swallowing fewer pills a lot easier.
Doctors like to use hydrochlorothiazide because it isn’t as harsh as some loop diuretics like furosemide. It doesn’t make you rush to the bathroom quite as much, and it’s less likely to throw your potassium levels into chaos. In the US, millions of prescriptions for hydrochlorothiazide are filled every year, so it’s far from rare.
Here’s a quick table showing how hydrochlorothiazide compares to furosemide in some common scenarios:
| Hydrochlorothiazide | Furosemide | |
|---|---|---|
| Mostly used for | High blood pressure, mild edema | Heavy swelling, heart/kidney issues |
| Potassium loss risk | Medium | High |
| Bathroom urgency | Lower | Higher |
This is the reason you’ll hear about hydrochlorothiazide for people with mild swelling or just stubborn high blood pressure—folks who don’t need a sledgehammer, just a nudge.
Pros
- Great for long-term blood pressure control
- Usually well-tolerated with fewer bathroom emergencies
- Often paired with other blood pressure meds (like ACE inhibitors or ARBs)
- Less risk of drastic potassium drops compared to furosemide
- Available as a cheap generic in almost every pharmacy
Cons
- Not strong enough for severe swelling, especially from heart or kidney problems
- Still can drop potassium (watch your blood work!)
- Might raise your blood sugar or cholesterol a bit
- Sometimes triggers gout attacks in those prone to them
- Effectiveness can fade if you have significant kidney disease
People often ask if they should just swap from furosemide to hydrochlorothiazide. It’s a solid option for lighter cases, but anyone with heart failure or big-time water retention will likely need more than what hydrochlorothiazide can deliver. Always double-check with your provider—they’ll match the right tool for the job.
Spironolactone
Spironolactone isn’t just another pill in the pharmacy drawer—it’s a powerful potassium-sparing diuretic, often recommended when furosemide alternatives are on the table. Doctors rely on it for patients with heart failure, fluid buildup from liver disease, or stubborn high blood pressure that hasn’t budged with thiazides. You might hear it called an 'aldosterone blocker'—that’s because it blocks a hormone that makes your body hold onto salt and water, driving the swelling down.
One huge perk here: unlike furosemide, spironolactone keeps your potassium from dipping too low. That makes it a solid pick if you've ever dealt with those twitchy muscles or weird heart flutters from other water pills. Some folks even see their blood pressure drop further when adding spironolactone to their routine—it’s been backed up by real-world data and guidelines in treating resistant hypertension.
Pros
- Protects potassium levels—great for avoiding cramps and dangerous drops.
- Especially useful in heart failure and liver cirrhosis where extra fluid is a headache.
- Often tacked on to other meds when standard diuretics aren’t enough.
- Can help lower blood pressure a notch further when the usual stuff isn’t cutting it.
Cons
- Hormonal side effects—think breast tenderness or growth (gynecomastia), especially at higher doses or with long-term use.
- If your kidneys already act up, risk of too much potassium is real. Regular blood tests are a must.
- May cause menstrual irregularities in women.
- Works slower than furosemide alternatives like loop diuretics. Don’t expect instant results if you’re really puffy.
Here’s a quick fact: The British National Formulary in 2024 estimated that about 25% of patients on high-dose spironolactone experience some kind of hormonal side effect. Still, if you’re careful about regular labs and open with your doctor about symptoms, most issues can be managed or avoided altogether.
Side-by-Side: Choosing the Right Alternative
If you’re weighing your options beyond regular furosemide alternatives, you’ll want a clear snapshot. Not every diuretic works the same, and what’s great for one person may cause headaches (sometimes literally) for someone else. Here’s how the main choices line up, so you can pick the best fit with your doctor.
| Medication | Best For | Biggest Pros | Common Cons |
|---|---|---|---|
| Amiloride | People with mild edema, high blood pressure, and those at risk of low potassium | Protects potassium, fewer hormonal side effects, decent for long-term use | Weak diuretic alone, risk of low sodium |
| Chlorthalidone | Stable blood pressure control | Lasts all day, proven for heart health | Can drop sodium or potassium, may raise blood sugar |
| Hydrochlorothiazide | High blood pressure, mild fluid retention | Widely used, gentle for most | May cause electrolyte shifts, less potent in kidney trouble |
| Spironolactone | Heart failure, resistant hypertension, conditions causing hormone imbalance | Protects potassium, can improve heart outcomes | Hormonal side effects, needs regular blood monitoring |
Here’s what makes a real difference:
- If keeping potassium up is top priority, amiloride and spironolactone are usually stronger picks than the rest.
- For people bothered by constant urination or blood pressure swings, chlorthalidone is a slow-and-steady option, good for all-day control.
- Those with kidney disease usually need a closer look with their doctor—some diuretics get weaker or riskier as kidney function changes.
- Regular blood tests matter. Potassium and sodium can sneak out of balance, especially with combo therapies. It’s worth asking your doc how often you’ll need labs.
Real talk: almost every furosemide alternative is about trading off power for fewer side effects. There’s no one-size-fits-all answer—just a smarter way to match your health issues, lab numbers, and daily life to the right option.



16 Comments
Eli Grinvald-25 April 2025
This is actually super helpful 😊 I’ve been on furosemide for years and my legs are always swollen, but the constant bathroom runs are killing me. Amiloride sounds like a dream-no more midnight marathons to the toilet. Thanks for breaking this down so clearly!
Josh Arce-25 April 2025
Wow so now we’re pretending diuretics are some kind of boutique skincare routine? Furosemide works. It’s cheap. It’s been around since the 60s. You want alternatives? Try drinking less water. Or better yet-don’t be a hypochondriac.
Alexis Hernandez-25 April 2025
Man, I love how this post doesn’t just throw meds at you but actually explains *why* you’d pick one over another. Like, I didn’t realize chlorthalidone lasts 72 hours-that’s wild. My uncle’s been on it for his BP and he says he forgets he’s even taking a pill. No more 3 PM bathroom emergencies. Also, spironolactone’s hormonal side effects? Yeah, that’s a real talk moment. My cousin stopped it because she started growing chest hair. Not a vibe.
But seriously, this is the kind of info docs should hand out instead of scribbling on a napkin. If you’re tired of feeling like a human coffee filter, this list is gold.
brajagopal debbarma-26 April 2025
So now instead of fixing your body you just swap one pill for another? Classic American medicine. In India we just eat bitter gourd and pray. Works better than all these fancy tables.
Carly Smith-27 April 2025
Why are you even talking about alternatives when the real problem is you eat too much salt? Just stop. You don’t need a new drug you need a new life. Also why is everyone so obsessed with potassium? It’s not a TikTok trend.
Kurt Stallings-28 April 2025
Diuretics. How quaint. The real solution is cellular hydration optimization via mitochondrial recalibration. But no, let’s keep playing with electrolyte roulette.
Angie Creed-29 April 2025
Let’s be real: furosemide isn’t the enemy. The system is. The pharmaceutical industry doesn’t want you to know that lifestyle changes work better than pills. But here we are, debating potassium levels like it’s a dating app swiping game. We’ve lost our way.
What if the real alternative isn’t amiloride… but self-awareness?
Michael Ferguson-30 April 2025
I’ve been on furosemide for 12 years and I’ve seen people come and go on these so-called alternatives. Most of them are just repackaged junk. Spironolactone gave my neighbor gynecomastia-he had to get surgery. Amiloride? Too weak. Chlorthalidone? Made his sugar spike. Hydrochlorothiazide? He got gout so bad he couldn’t walk. And now you’re telling me to just ‘trade off power for fewer side effects’? No. That’s not a trade. That’s surrender. The only thing that works is a low-sodium diet, daily walks, and prayer. Everything else is just corporate placebo with a fancy table.
And don’t get me started on the ‘regular blood tests’ nonsense. Who has time for that? My insurance won’t cover it. I’m not a lab rat. I’m a person trying to live.
So yeah, I’ll stick with furosemide. At least I know what I’m getting. At least it doesn’t make me feel like a woman with boobs I didn’t ask for. At least it doesn’t make me diabetic. At least it doesn’t cost $800 a month. You want alternatives? Fix the system. Don’t just sell me another pill.
And don’t tell me to ‘talk to my doctor.’ My doctor doesn’t even know what time it is anymore. He’s got 8 minutes per patient. He’s reading off a script. He’s not listening. So don’t act like this table is some kind of miracle. It’s just another distraction. We’re not solving anything. We’re just shuffling cards on a sinking ship.
And if you’re one of those people who thinks ‘potassium-sparing’ means you can eat Doritos all day? You’re not just wrong. You’re dangerous.
Caden Little- 1 May 2025
Y’all are overcomplicating this 😊 Seriously, if you’re dealing with swelling or high BP and furosemide’s wrecking your electrolytes, amiloride or chlorthalidone are legit swaps. I’ve helped a bunch of folks switch and the difference in energy levels is insane. Just make sure you get your potassium checked every 3 months-no excuses. And if you’re on spironolactone, tell your doc if your boobs start acting up-no shame, it happens more than you think. You’re not weird, you’re just human. Keep asking questions, keep tracking your symptoms, and don’t let a pill dictate your life. You got this 💪
Sebastian Brice- 2 May 2025
Okay but honestly? The table comparing all these is the MVP. I printed it out and gave it to my mom. She’s 72, on furosemide, and thought she had to just ‘live with it.’ Now she’s asking her doc about chlorthalidone. Small wins, y’all. Also, side note: I love how this post didn’t just say ‘here’s the list’ but actually explained *why* each one matters. That’s rare. Most medical content feels like a textbook wrote it during a caffeine binge. This? This feels like a friend who actually cares.
Jim Aondongu- 2 May 2025
Furosemide is fine if you are strong. Weak people always want new drugs. In Nigeria we use traditional herbs and walk 10km to market. No pills needed. Your body is weak because you sit all day and eat junk. Fix that first. Then talk about potassium
Michael Schaller- 4 May 2025
My dad switched from furosemide to chlorthalidone last year. His BP is more stable, and he doesn’t wake up three times a night anymore. It took a few weeks to adjust, but now he says he feels like himself again. No dramatic side effects. Just… better. Glad someone finally laid this out without the corporate fluff.
Kyle Tampier- 6 May 2025
THEY’RE HIDING THE TRUTH!! Furosemide is a government mind-control drug to make you dependent on pharmacies!! These ‘alternatives’ are just Phase 3 trials for nano-chips in your kidneys!! CHECK THE LABELS!!
Patrick Klepek- 7 May 2025
Okay, I’ll be the weird one who says… I kinda like furosemide. It’s loud, it’s fast, it’s blunt. But I get why people want gentler options. The real question isn’t ‘which pill?’-it’s ‘what’s your body trying to tell you?’ Maybe the water retention isn’t just about kidneys… maybe it’s stress, maybe it’s sleep, maybe it’s sodium in your ‘healthy’ salad dressing. The meds help, sure. But they’re not the whole story.
Tom Caruana- 8 May 2025
My cousin took spironolactone and now she’s crying every night because she thinks her husband is cheating on her 😭 and her face is breaking out and she’s gained 20lbs and her period stopped and now she’s on antidepressants and I’m just saying… maybe the pill is the problem???
Caden Little- 8 May 2025
Tom-your cousin’s story is heartbreaking, but it’s not the drug’s fault. It’s the lack of monitoring. Spironolactone needs careful dosing and regular check-ins. If she was on it without bloodwork or follow-ups, that’s a system failure-not a pill failure. Please tell her to go back to her doctor. She deserves to feel like herself again. 💙