Chemotherapy Drug Interaction Checker
Check for Dangerous Interactions
Enter your chemotherapy drug and any other medications, supplements, or foods you're taking to see potential interactions. Based on guidelines from the article.
Interaction Results
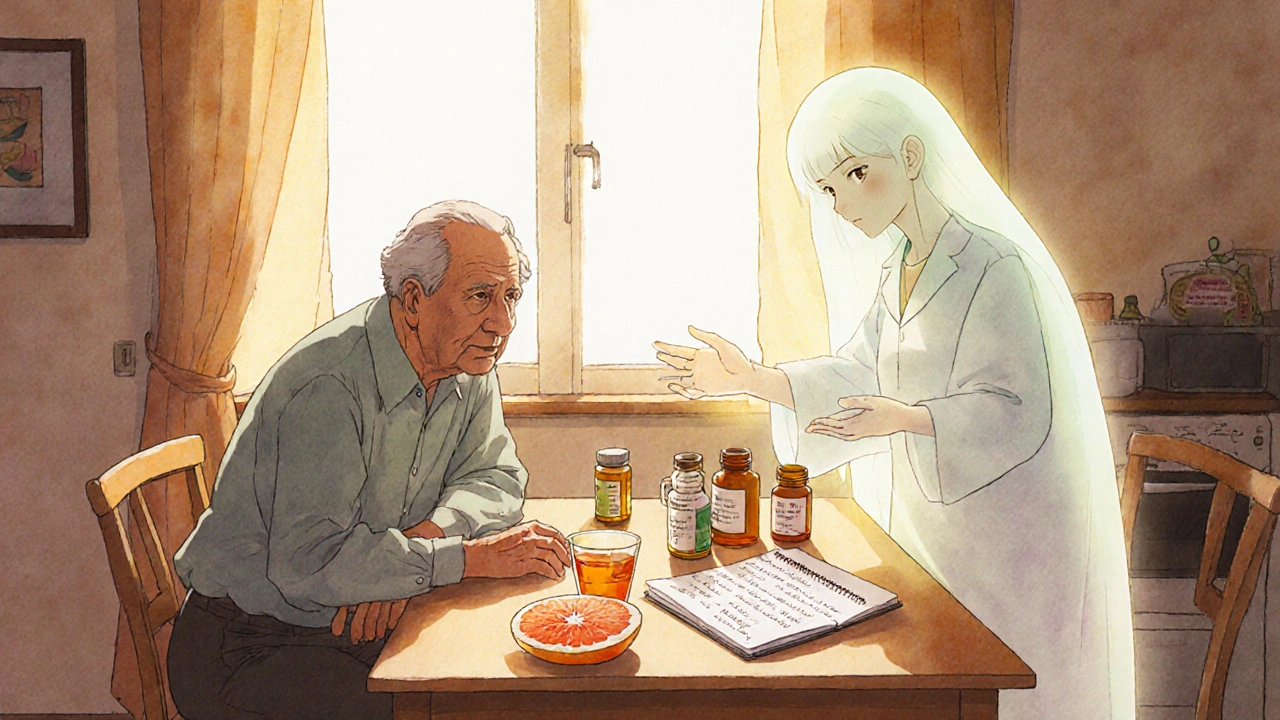
When you're undergoing chemotherapy, every pill, supplement, or even a glass of grapefruit juice can change how your treatment works. It’s not just about the cancer drugs themselves-it’s what they’re doing together with everything else you’re taking. Many patients don’t realize that common over-the-counter painkillers, herbal teas, or even vitamins can turn a safe treatment into a dangerous one. In fact, more than half of outpatient cancer patients experience at least one potential drug interaction, and one in three of those could lead to serious harm-like kidney damage, dangerous bleeding, or even treatment failure.
Why Chemotherapy Interactions Are So Dangerous
Chemotherapy drugs are powerful. They’re designed to kill fast-growing cells, but they don’t always know the difference between cancer cells and healthy ones. That’s why even small changes in how these drugs are absorbed, broken down, or cleared from your body can have big consequences. The most common type of interaction is pharmacokinetic-meaning one drug changes how your body processes another. This usually happens through the liver’s cytochrome P450 enzyme system, which handles about 70% of all medications. When two drugs compete for the same enzyme, one can slow down or speed up the other’s metabolism. For example, if a chemotherapy drug is broken down too slowly, it builds up and becomes toxic. If it’s broken down too fast, it doesn’t work at all.Common Culprits: Supplements and Foods That Interfere
Many people think natural means safe, but that’s not true with chemotherapy. Supplements like turmeric, ginger, ginkgo biloba, and fish oil can interfere with blood clotting, which is especially risky if you’re also on blood thinners or receiving treatments that lower platelets. Garlic and vitamin E can increase bleeding risk during surgery or after chemotherapy that affects bone marrow. Then there’s grapefruit-yes, that healthy breakfast fruit. It contains compounds called furanocoumarins that permanently block the CYP3A4 enzyme. That enzyme helps break down more than 50% of oral chemotherapy drugs, including etoposide, cyclophosphamide, and paclitaxel. One grapefruit can affect your body for days. Seville oranges and pomelos do the same thing. Even a single glass of juice can throw off your entire treatment schedule.Prescription Meds That Clash With Chemo
It’s not just supplements. Common prescription drugs can also cause problems. Antidepressants like paroxetine and fluoxetine can interfere with tamoxifen, a drug used for hormone-receptor-positive breast cancer. These antidepressants block the enzyme needed to turn tamoxifen into its active form, making it less effective. Studies show this interaction could increase recurrence risk. Pain relievers like ibuprofen and naproxen can increase the risk of kidney damage when taken with cisplatin or carboplatin. Even antibiotics like clarithromycin and antifungals like ketoconazole can dangerously raise levels of certain chemo drugs by blocking their breakdown. And don’t forget acid reducers-omeprazole and other PPIs can reduce the absorption of oral chemo drugs like dasatinib and nilotinib, making them less effective.The Rise of Oral Chemo and New Risks
More than 25% of chemotherapy drugs now come as pills you take at home. That means you’re managing your own treatment-and your own risks. Unlike IV chemo, which is given in a controlled setting with nurses watching for reactions, oral drugs are taken daily, often with other medications. This increases the chance of missed doses, wrong timing, or accidental combinations. It also means you’re more likely to be taking supplements, vitamins, or over-the-counter meds without telling your oncologist. A 2014 study of patients over 70 found that 75% had potential for serious interactions. Older adults are especially vulnerable because their liver and kidneys don’t clear drugs as efficiently. What was a safe dose at 50 might become toxic at 75.Immunotherapy Adds a Whole New Layer
Newer cancer treatments like immune checkpoint inhibitors (ICIs)-drugs like pembrolizumab and nivolumab-work differently. Instead of killing cancer cells directly, they help your immune system do it. But that also means they can trigger unusual reactions when mixed with other drugs. There are now documented cases where patients on ICIs developed severe liver damage or skin reactions like Stevens-Johnson Syndrome after taking common antibiotics or antivirals. These aren’t classic drug interactions-they’re immune-mediated. Your body starts attacking its own tissues because the immune system is overstimulated. This type of reaction wasn’t seen with traditional chemo, and it’s still poorly understood. Researchers are only beginning to map out which drugs might trigger these reactions, making it even more critical to tell your care team about every medication you’re taking.What You Can Do to Stay Safe
The best defense is knowledge and communication. Here’s what works:- Make a full list of everything you take: prescriptions, OTC meds, vitamins, herbs, teas, and even CBD or melatonin. Include dosages and how often you take them.
- Bring it to every appointment-even if you’ve given it before. Your list should be updated at every cycle.
- Ask your pharmacist to screen for interactions. Most hospitals now have oncology pharmacists who specialize in this. They use tools like Lexicomp or Micromedex to check for known risks.
- Avoid new supplements without approval. If you want to try something for fatigue or nausea, talk to your team first. There’s no such thing as a "safe" supplement during chemo unless it’s been reviewed.
- Stop grapefruit and Seville oranges entirely. No exceptions. Even occasional consumption can disrupt your drug levels for days.
- Don’t self-medicate for side effects. If you have pain, nausea, or trouble sleeping, ask your oncologist for approved options. What works for someone else might be dangerous for you.

When to Call Your Care Team Immediately
Some reactions need urgent attention. Contact your oncology team right away if you notice:- Unusual bruising or bleeding (nosebleeds, blood in urine or stool)
- Severe diarrhea or vomiting that doesn’t stop
- Sudden skin rash, blistering, or peeling
- Yellowing of skin or eyes (sign of liver stress)
- Swelling in your legs or shortness of breath (possible kidney or heart issue)
- Any new symptom that feels "off"-even if you think it’s unrelated
These aren’t normal side effects. They could be signs of a dangerous interaction. Don’t wait until your next appointment. Call today.
The Role of Your Care Team
Managing these interactions isn’t just your job-it’s the team’s responsibility too. Oncologists, pharmacists, and nurses should all be checking for interactions at every visit. But too often, communication gaps happen. A patient might tell their oncologist about their chemo but forget to mention the melatonin they started for sleep. Or their primary care doctor prescribes an antibiotic without knowing about the cancer treatment. That’s why having one person-usually a pharmacist-review your full medication list is essential. In fact, studies show that when pharmacists are involved in oncology care, the number of serious interactions drops by nearly 40%.What’s Next for Chemo Safety
The future of cancer treatment is personal. Researchers are now looking at how your genes affect how you process drugs. Some people naturally have slower or faster versions of the enzymes that break down chemotherapy. Genetic testing can now identify these differences before treatment starts. This means someday, your chemo dose might be adjusted based on your DNA-not just your weight or age. But until then, the safest approach is simple: be honest, be thorough, and never assume something is harmless. Your life depends on it.Can I take vitamins while on chemotherapy?
Some vitamins are okay, but many can interfere with chemo. High-dose antioxidants like vitamin C, E, and selenium may protect cancer cells from damage, reducing treatment effectiveness. Multivitamins are generally low-risk, but you should still tell your oncologist what you’re taking. Never start a new supplement without approval.
Is it safe to use CBD oil during chemotherapy?
CBD can interact with chemotherapy by affecting the same liver enzymes that process many chemo drugs. It may increase side effects like fatigue, nausea, or liver stress. There’s not enough research to say it’s safe, and most oncologists advise against it unless part of a monitored clinical trial.
Why can’t I take ibuprofen with my chemo?
Ibuprofen and other NSAIDs can increase the risk of kidney damage when combined with platinum-based chemo drugs like cisplatin or carboplatin. They can also raise bleeding risk if your platelets are low. Acetaminophen (Tylenol) is usually a safer choice for pain relief, but always check with your care team first.
Do all cancer drugs have the same interaction risks?
No. Traditional chemotherapy drugs have well-documented interaction profiles. Newer targeted therapies and immunotherapies have different risks. For example, immunotherapy can cause immune-related side effects when combined with certain antibiotics or antivirals, which didn’t happen with older chemo. Each drug has its own profile-there’s no one-size-fits-all answer.
How often should I review my medications with my oncologist?
At every visit-no exceptions. Even if nothing has changed, your body’s ability to process drugs can shift during treatment. Your liver and kidney function may decline, or you may start a new medication for a side effect. Always update your list and ask your pharmacist to check for interactions.


15 Comments
Shawn Daughhetee-24 November 2025
just took my chemo pills this morning and forgot i had a glass of grapefruit juice last night... now im sweating and paranoid
Miruna Alexandru-25 November 2025
the real tragedy isn't the drug interactions-it's that patients are expected to become pharmacologists overnight while their immune systems are being dismantled. the system doesn't care if you understand cytochrome P450-it just wants you to sign the consent form and show up for round two.
Justin Daniel-26 November 2025
man i used to think turmeric was magic until my aunt got her liver values through the roof after taking it with her chemo. now i just tell people: if it's not on your oncologist's approved list, treat it like a landmine. also-grapefruit is the devil's smoothie. no exceptions. ever.
Melvina Zelee-27 November 2025
so many people think natural = safe but like... my grandma took ginkgo biloba for her memory and ended up in the er with bleeding gums. turns out it thins blood like crazy. i told her she shoulda just eaten more blueberries. she said blueberries dont come in capsules so she didnt count them. i cried. then i made her a list. now she calls me before she takes anything. its weird but its working
steve o'connor-28 November 2025
the pharmacist at my hospital flagged a interaction between my chemo and my blood pressure med that my oncologist missed. i think that's why i'm still here. never underestimate the pharmacy team. they're the unsung heroes who read the fine print while everyone else is looking at the big picture.
ann smith-30 November 2025
you are NOT alone in this. every single person reading this has a team fighting for them-even if it doesn’t feel like it. 💪❤️ keep that list updated. call when something feels off. you’re doing better than you think.
Julie Pulvino- 2 December 2025
i used to take melatonin for sleep and didn’t think twice. then my oncologist said it might mess with my hormone therapy. so i stopped. slept worse for a week. then i started listening to audiobooks instead. weirdly better. point is: sometimes the fix isn’t another pill. it’s just changing the habit.
Daniel Jean-Baptiste- 3 December 2025
my dad took ibuprofen for his back pain and ended up with kidney issues. they had to delay his next chemo cycle. he said he thought it was just a regular painkiller. turns out nothing is regular when you're on chemo. now he uses heat packs and asks before he takes anything. learned the hard way
Jessica Correa- 5 December 2025
my sister started taking CBD for nausea and her chemo stopped working. they had to switch drugs. she didn't tell anyone because she thought it was herbal and harmless. dont be her. talk to your team. always
Nikhil Chaurasia- 6 December 2025
in india we have this saying: "if it is not prescribed by the doctor, it is poison." we don't have fancy tools like Lexicomp, but we have generations of wisdom. if your uncle took something and lived, that doesn't mean it's safe for you. your body is not his body. your cancer is not his cancer. listen to your oncologist, not your cousin's friend's aunt.
Holly Schumacher- 7 December 2025
you people are so naive. you think you're being proactive by taking "natural" supplements? you're just another statistic waiting to happen. the fact that you need a 3000-word article to understand that grapefruit ruins your treatment says everything about how broken our healthcare system is. you're not being careful-you're being lucky. and luck runs out.
Michael Fitzpatrick- 7 December 2025
when i was first diagnosed, i started taking vitamin D because i read it helps with immunity. then i found out it could interfere with my hormone therapy. i felt so stupid. but here's the thing-i didn't stop asking questions. i started bringing my entire medicine cabinet to every appointment. my oncologist laughed at first, then thanked me. now she says i'm her model patient. it's not about being perfect-it's about being honest. even when you feel silly for asking. even when you think it's "just a vitamin."
james lucas- 8 December 2025
my mom took omeprazole for heartburn and didn't realize it was making her chemo less effective. they had to redo her whole treatment plan. she said she didn't think it mattered because it was just for acid. but it mattered. a lot. now we have a whiteboard in the kitchen with all her meds and when to take them. and we check it together every morning. it's dumb but it works. and she's still here.
manish chaturvedi-10 December 2025
in my culture, we trust elders and traditional remedies. but when my father was undergoing treatment, we consulted both the oncologist and the Ayurvedic practitioner together. they sat in the same room and discussed interactions. it was the first time i saw modern medicine and tradition talk as equals. the result? no complications. no surprises. just care. you don't have to choose between worlds-you just have to make them talk to each other.
Patrick Marsh-11 December 2025
Don't. Take. Anything. Without. Asking.