Acne Treatment Finder
Find Your Best Acne Treatment
Answer a few questions to discover which treatment is best for your skin type, acne severity, and lifestyle.
When it comes to tackling stubborn acne, many people wonder whether a prescription like Cleocin is worth the hassle or if there’s a simpler solution out there. This guide breaks down Cleocin (clindamycin) side‑by‑side with the most common alternatives, so you can decide which option fits your skin type, budget, and lifestyle.
What is Cleocin?
Cleocin is a brand name for clindamycin phosphate 1% gel, a prescription‑only topical antibiotic used primarily for inflammatory acne. It works by stopping the growth of Propionibacterium acnes (now Cutibacterium acnes) and reducing inflammation. The gel is applied twice daily after cleansing and is often paired with a non‑comedogenic moisturizer.
Why compare alternatives?
Even though Cleocin is effective for many, it isn’t a one‑size‑fits‑all solution. Some patients experience dryness, antibiotic resistance, or simply want a non‑prescription route. By looking at the pros and cons of other treatments-both prescription and over‑the‑counter-you can avoid unnecessary side effects and possibly save money.
Key Decision Criteria
- Mechanism of action: Does it target bacteria, oil production, or inflammation?
- Formulation: Gel, cream, lotion, or oral tablet?
- Safety profile: Common side effects and contraindications.
- Cost and accessibility: Prescription required? Insurance coverage?
- Resistance risk: How likely is bacterial resistance to develop?
Top Alternatives to Cleocin
Below is a quick snapshot of the most frequently discussed options.
- Erythromycin is a topical antibiotic (often 2% solution) that also targets acne‑causing bacteria but tends to cause more irritation than clindamycin.
- Benzoyl Peroxide is an over‑the‑counter oxidizing agent that kills bacteria and exfoliates, available in 2.5‑10% creams, gels, and washes.
- Tretinoin is a prescription retinoid that speeds up cell turnover, reducing clogged pores and inflammation.
- Doxycycline is an oral tetracycline antibiotic taken once or twice daily, effective for moderate‑to‑severe inflammatory acne.
- Adapalene is a newer, OTC retinoid (0.1% gel) that balances efficacy with lower irritation compared to tretinoin.
- Azithromycin is an oral macrolide sometimes used off‑label for acne, with a shorter course than doxycycline.
- Tea Tree Oil is a natural essential oil with antibacterial properties, typically diluted to 5‑10% in a carrier oil.
Side‑by‑Side Comparison
| Treatment | Formulation | How It Works | Typical Use Cases | Main Pros | Main Cons |
|---|---|---|---|---|---|
| Cleocin (Clindamycin) | 1% gel (prescription) | Inhibits bacterial protein synthesis | Mild‑to‑moderate inflammatory acne | Targeted antibacterial action, low irritation for most users | Antibiotic resistance risk, requires prescription |
| Erythromycin | 2% solution or gel (prescription) | Blocks bacterial protein synthesis | Similar acne severity as Cleocin | Effective against resistant strains when combined with benzoyl peroxide | Higher rates of skin irritation, also resistance prone |
| Benzoyl Peroxide | 2.5‑10% cream, gel, wash (OTC) | Oxidizes bacterial membranes; keratolytic | Mild‑to‑moderate acne, often as adjunct therapy | No resistance development, fast action | Dryness, bleaching of fabrics, can sting sensitive skin |
| Tretinoin | 0.025‑0.1% cream or gel (prescription) | Stimulates cell turnover, reduces follicular plugging | Comedonal and inflammatory acne | Improves texture, reduces post‑inflammatory hyperpigmentation | Initial irritation, photosensitivity |
| Doxycycline | 100mg oral tablet (prescription) | Inhibits bacterial protein synthesis; anti‑inflammatory | Moderate‑to‑severe inflammatory acne | Systemic control of deep lesions, works quickly | Photosensitivity, GI upset, potential gut flora disruption |
| Adapalene | 0.1% gel (OTC) | Selective retinoid receptor agonist | Comedonal and inflammatory acne | Lower irritation than tretinoin, available without prescription | May take several weeks to see results |
| Tea Tree Oil | 5‑10% diluted in carrier (OTC) | Disrupts bacterial cell walls | Mild acne, spot treatment | Natural, inexpensive, low systemic risk | Potential for allergic dermatitis, less potent than pharmaceuticals |
When Cleocin Is the Better Choice
If you’ve tried benzoyl peroxide or OTC retinoids and still have persistent red bumps, Cleocin can be a game‑changer. Its targeted antibacterial effect works well when the primary issue is inflammation caused by bacterial overgrowth. It also pairs nicely with benzoyl peroxide-using them together reduces the chance of resistance while still keeping side effects manageable.
Scenarios Where Alternatives Shine
Consider the following situations:
- Dry or Sensitive Skin: Benzoyl peroxide or oral antibiotics may aggravate dryness. A gentle retinoid like adapalene or a natural option such as tea tree oil can be kinder.
- Severe Nodular Acne: Topical therapy alone often falls short. Oral doxycycline or a combination of oral and topical agents is usually recommended.
- Pregnancy: Many oral antibiotics and retinoids are contraindicated. Cleocin is generally considered safe in pregnancy (Category B), but always confirm with a healthcare provider.
- Budget Constraints: OTC benzoyl peroxide and adapalene cost far less than a monthly prescription for Cleocin.
- Concern About Antibiotic Resistance: Rotating to non‑antibiotic options like benzoyl peroxide or retinoids can mitigate the risk.
How to Combine Treatments Safely
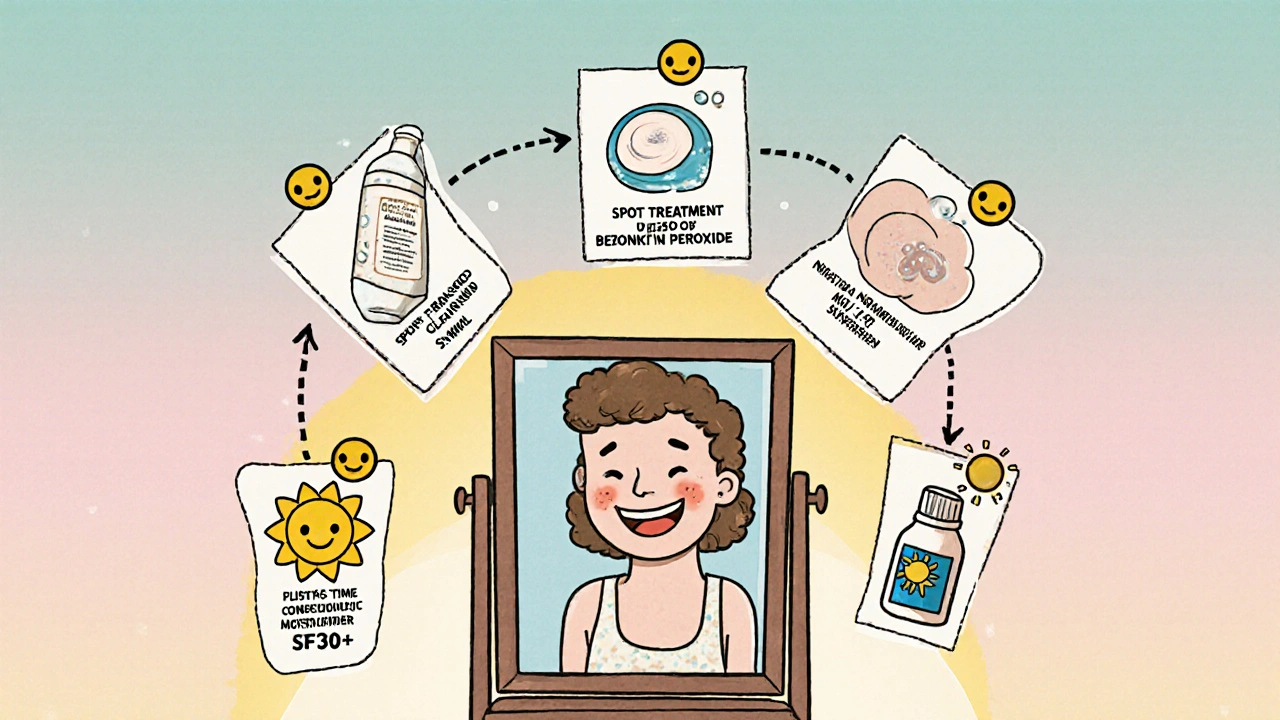
Most dermatologists recommend a “layering” approach:
- Cleanser: Use a gentle, pH‑balanced cleanser morning and night.
- Spot Treatment: Apply benzoyl peroxide (2.5%) to active pimples only.
- Prescription Gel: Apply Cleocin to the entire affected area after the benzoyl peroxide has dried (wait ~5minutes).
- Moisturizer: Choose a non‑comedogenic, fragrance‑free moisturizer to combat dryness.
- Sunscreen: Finish with SPF30+ daily; retinoids and antibiotics both increase photosensitivity.
Never use multiple strong actives (e.g., benzoyl peroxide + a high‑strength retinoid) at the same time unless your dermatologist advises a gradual build‑up.
Cost Snapshot (2025 Australia)
- Cleocin 30g tube - approx. AUD45-55 (PBS subsidized for eligible patients).
- Erythromycin 30g - similar price to Cleocin, often not PBS listed.
- Benzoyl Peroxide 30ml - AUD12-18 (OTC).
- Tretinoin 20g - AUD30-45 (prescription).
- Doxycycline 28 tablets - AUD15-25 (PBS subsidized).
- Adapalene 30g - AUD20-25 (OTC).
- Tea Tree Oil 10ml - AUD8-12 (OTC).
Potential Pitfalls & How to Avoid Them
- Over‑dryness: Start with a low concentration benzoyl peroxide and build up. Pair with a rich but non‑comedogenic moisturizer.
- Resistance Development: Use Cleocin for no longer than 12weeks unless a dermatologist says otherwise. Rotate with benzoyl peroxide or retinoids.
- Allergic Reaction: Patch‑test new products on the inner forearm for 48hours before full‑face use.
- Sun Sensitivity: Apply sunscreen every morning, even on cloudy days, especially if you’re using doxycycline or retinoids.
Bottom Line: Personalize Your Regimen
There’s no universal "best" acne drug. Cleocin shines when bacterial inflammation is the main culprit and you want a prescription‑strength, but low‑irritation topical. If you’re dealing with oily, comedonal acne, a retinoid or benzoyl peroxide may give you quicker results. For severe, deep lesions, oral antibiotics like doxycycline become necessary.
Talk to a dermatologist, consider your skin type, budget, and how long you’re willing to stay on a medication. A tailored mix-perhaps benzoyl peroxide in the morning, Cleocin at night, and a moisturizer in between-often delivers the clearest skin without the drama.
Frequently Asked Questions
Can I use Cleocin and benzoyl peroxide together?
Yes, but apply them at different times of day. Benzoyl peroxide in the morning, let it dry, then apply Cleocin at night. This sequence reduces irritation and prevents the antibiotic from being inactivated by the peroxide.
How long should I stay on Cleocin?
Most dermatologists recommend 8-12weeks. Extending beyond that raises the risk of bacterial resistance, so a break or switch to a non‑antibiotic maintenance therapy is advised.
Is Cleocin safe during pregnancy?
Cleocin is classified as Category B in Australia, meaning animal studies haven’t shown risk and there are no well‑controlled human studies. It’s generally considered safe, but you should always get your doctor’s final say.
Why did my acne get worse after starting Cleocin?
A short flare‑up, known as the “purge,” can happen when bacteria die off rapidly. It typically resolves within 2-4weeks. If redness persists beyond that, talk to your dermatologist about adjusting the regimen.
Can I replace Cleocin with an over‑the‑counter product?
For mild acne, an OTC benzoyl peroxide or adapalene regimen may suffice. However, if bacterial inflammation is dominant, an antibiotic like Cleocin usually works faster and more effectively.




18 Comments
Elle Trent-15 October 2025
Honestly, the pharmacodynamics of Cleocin are just a superficial patch for the deeper microbiome dysbiosis that topical antibiotics inevitably cause. You’re basically swapping one opportunistic strain for another, all while pumping your skin with a synthetic peptide that offers limited penetration. The literature shows a modest 10‑15% improvement over baseline, which is hardly a breakthrough when you factor in the resistance cascade. If you’re chasing flawless skin, you might as well invest in a robust barrier repair regimen first.
Jessica Gentle-16 October 2025
Let’s break this down step by step so everyone can follow along, regardless of where they are on their acne journey. First, Cleocin’s mechanism-targeting Cutibacterium acnes via protein synthesis inhibition-makes it a solid option for inflammatory lesions, especially when those lesions are resistant to benzoyl peroxide alone. Second, the risk of antibiotic resistance is real, but it can be mitigated by using Cleocin for a finite period (typically 8‑12 weeks) and pairing it with a non‑antibiotic like benzoyl peroxide to reduce bacterial load.
Third, consider skin type: oily, acne‑prone skin often tolerates the mild dryness from a 1% gel better than dry, sensitive skin, which may flare with any antibiotic. For the latter, a gentler retinoid such as adapalene or a soothing niacinamide serum might be preferable.
Fourth, cost and accessibility matter. In many regions, Cleocin is subsidized, but the out‑of‑pocket expense can still be a barrier compared to OTC options like a 5% benzoyl peroxide wash.
Fifth, pregnancy safety is a common concern. Cleocin is Category B, meaning it’s generally considered safe, but a dermatologist’s guidance is essential.
Sixth, layering strategy: start with a gentle cleanser, wait a few minutes after applying benzoyl peroxide, then apply Cleocin, followed by a non‑comedogenic moisturizer and SPF. This sequence minimizes irritation and maximizes efficacy.
Seventh, monitor for the “purge” phase-initial worsening is normal as the bacterial die‑off can provoke inflammation for 2‑4 weeks.
Eighth, if you notice persistent dryness, introduce a ceramide‑rich moisturizer to restore barrier function.
Ninth, always patch‑test new products to avoid allergic reactions.
Tenth, keep a simple skincare log: note product, time of day, and any side effects. This helps you and your dermatologist adjust the regimen quickly.
Eleventh, remember that diet and lifestyle-adequate hydration, balanced nutrition, and stress management-play supportive roles in skin health.
Twelfth, if after 12 weeks you see minimal improvement, discuss switching to an oral option like doxycycline or a stronger retinoid with your doctor.
Finally, be patient. Acne treatments often require 8‑12 weeks to show meaningful results, and consistency is key. With the right combination of Cleocin, adjunctive therapies, and good skincare habits, many people achieve clearer skin without the drama of severe side effects.
Samson Tobias-17 October 2025
Hey there, I totally get how overwhelming the options can feel, especially when your skin seems to be on a roller‑coaster. If you’re leaning toward Cleocin, start slow-apply it every other night and watch how your skin reacts. Pair it with a fragrance‑free moisturizer to keep the barrier happy, and don’t forget sunscreen; both antibiotics and retinoids can increase photosensitivity. Should you notice excess dryness, a gentle hyaluronic acid serum can be a lifesaver. Remember, consistency beats intensity every time.
Alan Larkin-18 October 2025
Mate, you’re over‑complicating this – just slap on a 2.5% benzoyl peroxide in the morning, let it dry, then pop Cleocin at night. It’s the classic 2‑step combo that actually works for most folks. No need to reinvent the wheel. 😎
Mike Brindisi-19 October 2025
cleocin is ok but i think you should try adapalene its less irritating and works well with benzoyl peroxide also it’s cheaper and you dont need a prescription
Abhishek Vernekar-20 October 2025
While I appreciate the enthusiasm for Cleocin, the syntax in many posts tends to misuse commas and semicolons – a properly punctuated sentence would read: “Cleocin, when used correctly, can reduce inflammatory lesions effectively.” Also, note the British spelling of “behaviour” if you’re targeting an international audience. Small details matter in medical writing.
Zachary Endres-21 October 2025
Wow, this guide is a ray of sunshine! 🌞 I love how it balances science with real‑world tips. For anyone on the fence, think of Cleocin as your reliable sidekick when the acne villains get too aggressive. And if you’re scared of dryness, a buttery moisturizer can turn that sidekick into a superhero. Keep the faith, your skin will thank you!
Ashley Stauber-22 October 2025
Honestly, I think the whole “Cleocin is the best” hype is just marketing fluff. Most of us can get away with cheap OTC stuff if we’re disciplined enough. No need to waste money on prescriptions when a simple benzoyl peroxide wash does the trick.
Amy Elder-23 October 2025
Great info.
Erin Devlin-24 October 2025
Clarity arises when we stop treating acne as a curse and see it as a signal.
Will Esguerra-25 October 2025
One must meticulously evaluate the pharmacokinetic profile of clindamycin before endorsing its widespread use. The specter of bacterial resistance looms large, and without judicious rotation of therapeutic agents, we risk ushering in an era of recalcitrant acne. Moreover, the dermal barrier disruption observed in a subset of patients cannot be dismissed as trivial; it may precipitate a cascade of secondary infections. Therefore, I implore clinicians to adopt a measured, evidence‑based approach, integrating Cleocin only when warranted by robust clinical indicators.
Priya Vadivel-26 October 2025
Thank you for this thorough breakdown! 😊 I especially appreciate the clear layering steps-cleanse, benzoyl peroxide, Cleocin, moisturizer, sunscreen. That sequence really helps demystify the routine. Also, the tip about patch‑testing new products is something many of us overlook; it can prevent a lot of unnecessary irritation. Lastly, the cost comparison table is incredibly useful for budgeting, especially when considering PBS subsidies. Great job making this both scientific and practical!
Dharmraj Kevat-27 October 2025
Okay look the drama around Cleocin is overblown don’t get scared just try it with a low dose and see how it goes
Navjot Ghotra-28 October 2025
cleocin works but its not magic it needs a good routine otherwise you’ll see no difference
parag mandle-29 October 2025
From a clinical standpoint, Cleocin offers a targeted antibacterial effect, yet its efficacy is amplified when combined with a keratolytic agent such as benzoyl peroxide. This synergistic approach not only curbs resistance development but also addresses comedonal lesions that antibiotics alone cannot resolve. Remember, adherence to a consistent regimen is the linchpin of success.
Shivali Dixit Saxena-30 October 2025
Hey! If you’re new to this, start with a gentle cleanser, then apply a pea‑sized amount of Cleocin at night, and finish with a moisturiser that contains ceramides. Don’t forget SPF during the day! 🌞 This simple routine has helped many people keep breakouts under control without feeling like they’re using a chemistry lab on their face.
Sayam Masood-31 October 2025
One might argue that the very act of medicating the skin reflects a deeper desire to control the uncontrollable, a paradox that underlies much of modern dermatology. Yet, in practice, the choice between Cleocin and its alternatives often hinges on personal tolerance and philosophical acceptance of imperfection.
Jason Montgomery- 1 November 2025
Good rundown! If you’re feeling stuck, try mixing up the schedule a bit-maybe Cleocin every other night and keep the benzoyl peroxide daily. It keeps things fresh and can reduce irritation over time.