Colchicine Antibiotic Interaction Checker
Check Your Medication Risk
This tool helps you determine if your medications can cause dangerous toxicity when taken together.
Imagine taking colchicine for gout or heart inflammation, then getting prescribed clarithromycin for a sinus infection. Sounds routine, right? But this combo can land you in the ICU. It’s not rare. It’s not theoretical. It’s happening right now in hospitals and clinics across the U.S., and most doctors don’t see it coming.
Why This Interaction Is So Dangerous
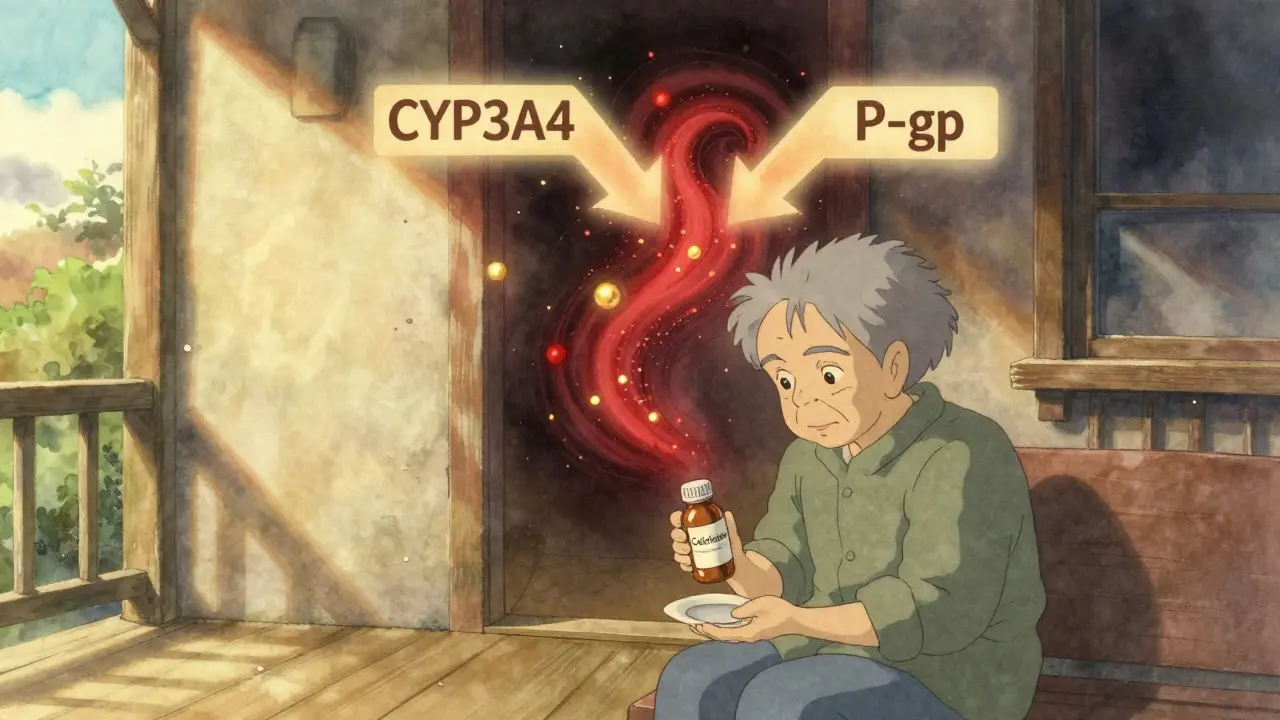
Colchicine isn’t your average pill. It’s powerful, with a razor-thin line between helping and harming. At normal doses, it stops gout flares and reduces heart inflammation. But when its levels rise just a little too much, it starts attacking your cells-muscles, bone marrow, organs. Toxicity can mean muscle breakdown, low white blood cells, organ failure, even death. The problem isn’t colchicine alone. It’s what happens when it meets certain antibiotics, especially macrolides like clarithromycin and erythromycin. These drugs don’t just sit beside colchicine-they actively trap it inside your body. Here’s how: colchicine relies on two cleanup systems to stay safe. One is CYP3A4, a liver enzyme that breaks it down. The other is P-glycoprotein (P-gp), a transporter that kicks it out of cells in your gut, liver, and kidneys. When you take a macrolide like clarithromycin, it blocks both systems at once. No breakdown. No exit. Colchicine piles up. Concentrations can jump four times higher than normal. That’s not a typo. Four times.Not All Macrolides Are the Same
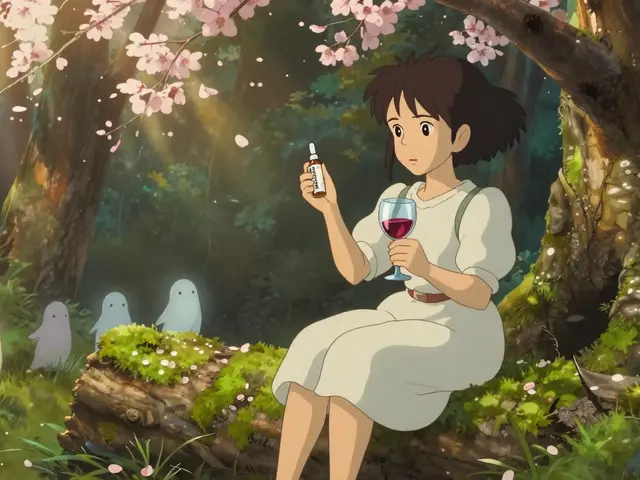
You might think all macrolides act the same. They don’t. Azithromycin? Safe. Clarithromycin? Dangerous. Erythromycin? Risky, but less so. Why? Because their ability to block CYP3A4 and P-gp varies. Clarithromycin is a double threat-it shuts down CYP3A4 with an IC50 of 1.6 μM and P-gp at 12.7 μM. That’s strong. Erythromycin is weaker on both. Azithromycin? Barely touches either. A 2022 study of over 12,000 patients showed azithromycin didn’t raise colchicine toxicity risk at all. Clarithromycin? It tripled the risk. This isn’t academic. In real-world ERs, 63% of colchicine toxicity cases tied to macrolides involved clarithromycin. Only 28% involved erythromycin. And azithromycin? Nearly zero. So if you need an antibiotic while on colchicine, azithromycin isn’t just an option-it’s the standard of care.What Else Can Make This Worse?
Clarithromycin isn’t the only culprit. Other drugs can trigger the same deadly combo:- Verapamil (a blood pressure drug)
- Diltiazem (another heart med)
- Amiodarone (for irregular heartbeat)
- Ketoconazole and itraconazole (antifungals)
- Ritonavir and other HIV protease inhibitors
Who’s at Highest Risk?
Not everyone who takes this combo gets sick. But some are sitting ducks:- Older adults (over 65)
- People with kidney problems
- Those on higher colchicine doses (like 0.6 mg twice daily)
- Patients taking multiple interacting drugs

Real Cases, Real Consequences
In 2019, a group of 12 patients were admitted with severe colchicine toxicity after taking clarithromycin. All were on standard doses. All developed neutropenia. Several had rhabdomyolysis. Three died. The FDA’s adverse event database from 2015 to 2020 recorded 147 such cases. Most involved clarithromycin. Many were preventable. A 2023 survey of 245 doctors found that 68% had seen at least one case. Emergency room physicians saw them more often-82% compared to 54% of rheumatologists. Why? Because ER docs see the aftermath. Rheumatologists often prescribe colchicine, but don’t always know what antibiotics their patients are getting from other doctors. And here’s another blind spot: patients don’t always tell their doctors about over-the-counter supplements. St. John’s wort, grapefruit juice, even some herbal remedies can inhibit CYP3A4. No one asks. No one thinks to check.What Should You Do?
If you’re on colchicine, here’s your action plan:- Never take clarithromycin or erythromycin unless there’s no alternative.
- Ask for azithromycin instead. It works just as well for most infections and doesn’t interfere.
- If you must take a high-risk drug, reduce your colchicine dose by 50%. For example, drop from 0.6 mg twice daily to 0.3 mg once daily.
- Get your kidney function checked regularly. If your eGFR is below 60, you’re already at higher risk.
- Tell every doctor you see that you’re on colchicine. Even if they’re prescribing a new medication for something unrelated.
Why Aren’t Doctors Catching This?
It’s not that they’re careless. It’s that the system fails them. Most electronic health records don’t warn you clearly. Even when they do, alerts are buried under dozens of other pop-ups. A 2024 study showed that when Epic updated its alert system to be more specific-highlighting clarithromycin as a top-tier danger-prescribing errors dropped by 63%. Also, many doctors still think, “It’s just an antibiotic. How bad could it be?” But colchicine isn’t like statins or blood pressure pills. It’s not forgiving. One wrong combo, and the damage can be irreversible.
What’s Changing? What’s Next?
The good news? Things are improving. Takeda, the maker of colchicine, is testing a new version-COL-098-that doesn’t rely on P-gp. Early trials show it’s 92% less likely to interact with clarithromycin. That could be a game-changer. Genetic testing is also becoming more practical. A 2023 study found that two gene variants-CYP3A5*3/*3 and ABCB1 3435C>T-predicted 78% of toxicity cases. If you have these, you’re at much higher risk. Soon, we may test for them before prescribing colchicine. Right now, the best defense is awareness. Know the drugs. Know your kidneys. Know your alternatives.Frequently Asked Questions
Can I take azithromycin with colchicine?
Yes. Azithromycin does not significantly inhibit CYP3A4 or P-gp, and large studies show it doesn’t raise colchicine levels or increase toxicity risk. It’s the safest macrolide choice if you need an antibiotic while on colchicine.
Is it safe to take clarithromycin if I lower my colchicine dose?
No. Even with a 50% dose reduction, clarithromycin can still push colchicine levels into the toxic range. The interaction is too strong and unpredictable. Avoid the combination entirely. Choose azithromycin instead.
What symptoms should I watch for if I accidentally took both?
Watch for muscle pain or weakness, especially if it’s sudden. Also watch for fever, fatigue, unexplained bruising, or frequent infections-these can signal low white blood cells. Nausea, vomiting, or diarrhea may come on quickly. If you experience any of these after taking both drugs, seek medical help immediately.
Do grapefruit juice or St. John’s wort interact with colchicine?
Yes. Grapefruit juice strongly inhibits CYP3A4. St. John’s wort can inhibit both CYP3A4 and P-gp. Even if you’re not on a macrolide, these can still raise colchicine levels. Avoid them completely while taking colchicine.
Is there a blood test to check colchicine levels?
Yes, but it’s not widely available. Only about 37% of U.S. hospitals can run a colchicine level test. It’s used mainly in critical cases or research settings. Don’t rely on it for routine safety-prevention through drug selection is far more effective.
Why is colchicine still used if it’s so dangerous?
Because when used correctly, it’s one of the most effective and affordable treatments for gout, pericarditis, and heart inflammation after a heart attack. It costs about $4,200 a year-compared to $198,000 for alternatives like canakinumab. The risk is real, but manageable with the right precautions.


5 Comments
Natasha Plebani-30 January 2026
Colchicine’s pharmacokinetics are a masterclass in narrow therapeutic windows. The dual inhibition of CYP3A4 and P-gp by clarithromycin isn’t just a drug interaction-it’s a pharmacodynamic cascade. The 4-fold plasma concentration spike isn’t linear; it’s exponential due to saturation kinetics in hepatocytes and renal tubular cells. This isn’t a ‘watch out’-it’s a systems failure waiting to happen in polypharmacy patients. The real tragedy? We’re still treating this like a footnote when it should be a red flag in every EHR algorithm.
Eliana Botelho-31 January 2026
Okay but have you considered that maybe the whole ‘colchicine danger’ thing is just Big Pharma scaremongering to sell more expensive alternatives? Like, I read this study that said 90% of toxicity cases were in people who were also drinking grapefruit juice and taking St. John’s wort and didn’t tell their doctor-so why blame the antibiotic? Also, my cousin took clarithromycin with colchicine and lived to tell about it. Maybe it’s not that bad? 🤷♀️
Darren Gormley- 1 February 2026
Clarithromycin = 🚨
Azithromycin = ✅
Colchicine = 💣
Doctors = 😴
Patients = 💀
System = 🤡
Why are we still having this conversation in 2025? The data’s been out since 2020. If your EHR doesn’t scream ‘DANGER’ when you type ‘clarithromycin’ next to ‘colchicine’, you’re not a doctor-you’re a liability.
Mike Rose- 1 February 2026
bro i just took clarithro and colchicine last week and im fine lmao. why u so scared? its just a pill. my grandma took it for 10 years. they just wanna scare you so u buy the expensive azithro. 💩
Russ Kelemen- 2 February 2026
This is exactly why we need better communication between specialists. I’ve seen patients on colchicine for pericarditis get antibiotics from urgent care without any cross-check. The solution isn’t just ‘avoid clarithromycin’-it’s building systems. Pharmacist-led med reconciliations. Automated alerts that don’t get buried. Patient handouts in plain language. We can fix this. But it takes intentionality. You’re not just prescribing drugs-you’re managing risk. And this risk? It’s silent until it’s too late.