Managing medications at home can be overwhelming-especially for older adults taking five, ten, or even more pills a day. Missed doses, wrong times, duplicate prescriptions, and dangerous interactions happen more often than people realize. In fact, medication errors cause about 30% of all adverse events in home care. But there’s a proven solution: home health services designed specifically for medication management. These services don’t just hand out pills-they help prevent hospital trips, reduce confusion, and give families peace of mind.
What Home Health Services Actually Do for Medication Management
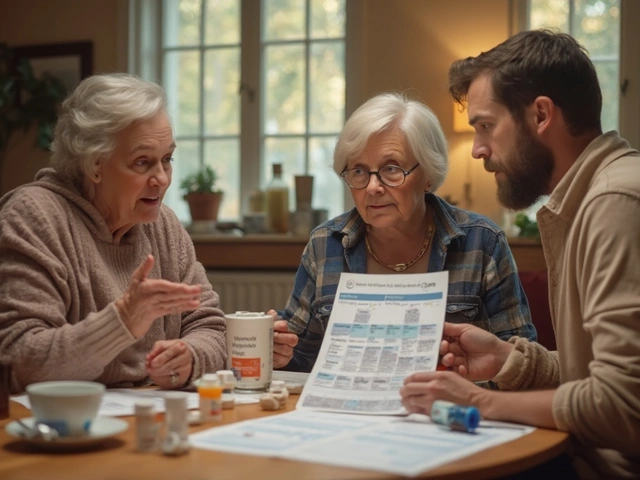
Home health services for medication management go far beyond reminding someone to take their pills. They’re a full system built around safety, accuracy, and continuity of care. A trained nurse or medication aide visits the home and follows a strict protocol: they check every medication against the latest doctor’s orders, verify dosages, confirm allergies, and make sure nothing’s being duplicated or conflicting. These professionals also update the patient’s official medication list-what’s called a medication reconciliation. This list includes every drug: prescription, over-the-counter, vitamins, and supplements. It lists the brand name, generic name, dose, frequency, reason for taking it, and any known side effects. This list gets shared with every doctor, pharmacist, and specialist involved in the patient’s care. Without this step, it’s easy for one doctor to prescribe something that clashes with another’s prescription. According to Clarest’s 2023 data, patients using professional medication management saw a 20% drop in 30-day hospital readmissions. That’s not a small number-it means fewer emergency visits, fewer complications, and more time spent safely at home.Tools That Make Medication Management Easier
No one can remember ten different schedules. That’s where tools come in. The most effective ones are simple, visual, and reliable. Pill organizers are a game-changer. Studies show they reduce medication errors by up to 45%. Look for ones with compartments for morning, afternoon, evening, and bedtime. Some even have alarms built in. But don’t just buy any organizer-make sure it matches the patient’s exact regimen. A weekly organizer won’t help if someone needs to take a pill three times a day. Phoenix Home Care’s WellPack system takes this further. Instead of a plastic box, they use pre-filled daily pouches. Each pouch has all the pills for that day, labeled clearly with the time and purpose. No counting, no guessing. Just open and take. For patients with dementia or vision problems, this is life-changing. Digital tools help too. Smartphone apps with alarms and reminders improve adherence by 35%. Some newer apps even let caregivers get alerts if a dose is missed. CritiCare’s 2023 app added biometric verification-patients must scan their fingerprint or face to confirm they took the pill. That cut administration errors by 40% in pilot programs.Who Qualifies for Home Health Medication Services?
Not everyone can get these services for free. Medicare Part A covers them-but only under strict conditions. You must be homebound, have a doctor’s order, and need skilled nursing care. That means if someone just needs help remembering to take pills, Medicare won’t pay. But if they’ve been discharged from the hospital after a stroke, heart surgery, or infection, and they need a nurse to check their meds, monitor for side effects, and coordinate with doctors, then yes-they qualify. For those who don’t meet Medicare’s criteria, private home care agencies offer medication management as a paid service. Prices range from $20 to $40 per hour, depending on location and complexity. That adds up quickly if someone needs daily help. Some Medicaid waiver programs cover this for low-income seniors, but eligibility varies by state. AARP reports that 62% of adults over 85 use home health medication services, compared to just 28% of those aged 65-74. The older you are, the more likely you are to need this support. It’s not about age alone-it’s about how many medications you’re taking and whether you’re managing them safely.How Medication Management Reduces Risk
Polypharmacy-taking five or more medications-is common among seniors. But it’s also dangerous. Each extra pill increases the chance of side effects, interactions, or confusion. Professional services catch problems before they become emergencies. Phoenix Home Care reviewed 200 patients over six months. Their nurses found duplicate prescriptions in 12 cases-like two different doctors prescribing the same blood thinner. One case could have caused internal bleeding. Another patient was taking a painkiller that clashed with their heart medication, leading to dizziness and falls. Both were caught before harm happened. The American Geriatrics Society recommends using the Beers Criteria-a list of medications that are risky for older adults. Home health nurses are trained to spot these. If a patient is on an anticholinergic drug like diphenhydramine (Benadryl) for sleep, the nurse will flag it. These drugs can cause confusion, memory loss, and increased fall risk in seniors. A safer alternative might be available. MedPro’s 2022 analysis found that professional management reduces adverse drug events by 60% compared to self-management. That’s the difference between staying at home and ending up in the ER.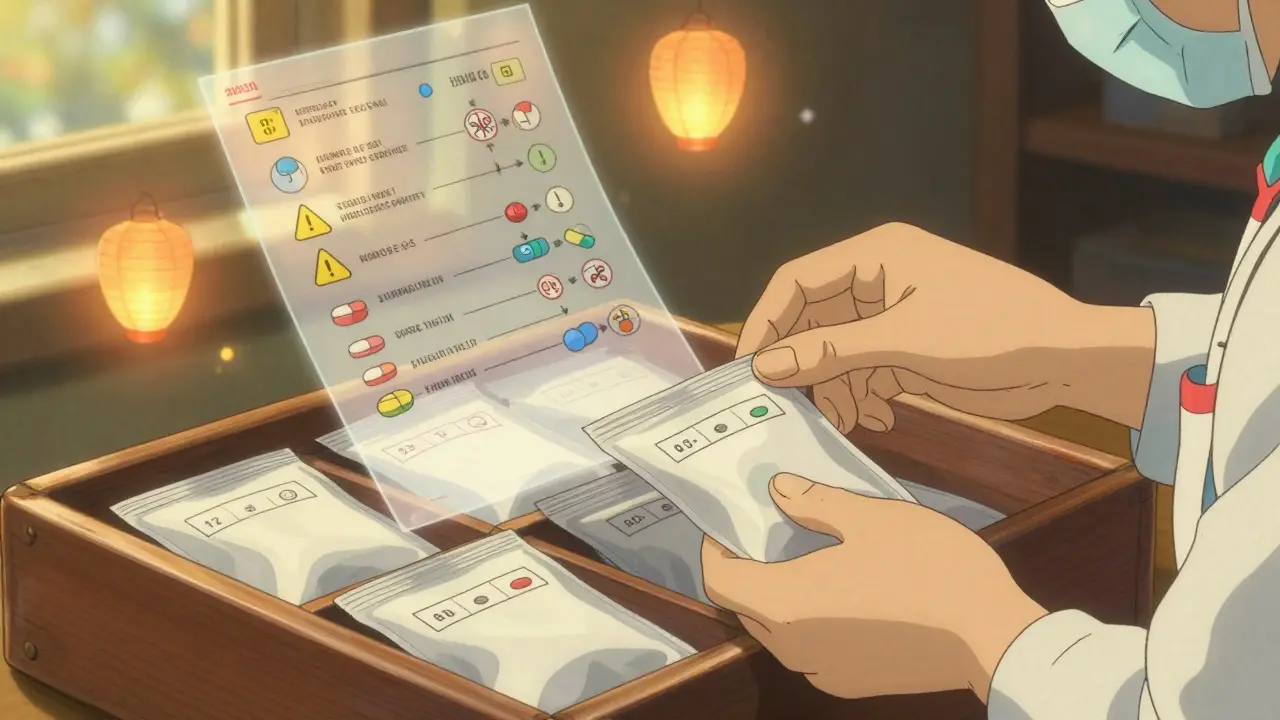
What to Expect During the First Visit
The first visit is a full assessment. It’s not just about handing out pills-it’s about understanding the whole picture. A skilled nurse will:- Review every prescription, including OTCs and supplements
- Check for duplicates or conflicting drugs
- Verify insurance coverage and cost
- Explain each medication’s purpose in simple terms
- Use the teach-back method: ask the patient to explain it back
- Set up a visual schedule-large print, color-coded, in their preferred language
- Confirm emergency contacts and action plans
Real Stories: What Works and What Doesn’t
Mary K. from Ohio used Phoenix Home Care’s WellPack system for her mother with Alzheimer’s. Before, her mother missed 30% of her doses. Within two weeks, missed doses dropped to under 5%. “It’s like someone else was watching over her,” Mary said. But not all experiences are smooth. John T. from Reddit shared a scary story: his father was on warfarin, a blood thinner. A new doctor prescribed aspirin without checking the list. The two drugs together caused internal bleeding. John’s father ended up in the ER. The problem? No one had a current, shared medication list. A Clarest survey of 500 caregivers found 78% saw better adherence with professional help. But 42% struggled with coordinating between multiple doctors. One patient had six different prescribers. No one talked to each other. The home health nurse became the central hub-collecting updates, calling doctors, and making sure everyone was on the same page.How to Get Started
If you’re considering home health services for medication management, here’s how to begin:- Ask the patient’s primary doctor for a referral. They must order the service for Medicare to cover it.
- Call local Medicare-certified home health agencies. Ask if they offer medication management as part of their care plan.
- For private pay, search for agencies with trained medication aides-not just companions or personal care workers.
- Ask about their process: Do they use reconciliation? Do they update the list? Do they use visual aids?
- Request a trial visit. See how they interact with the patient. Are they patient? Clear? Detailed?
- Confirm they document changes within 24 hours and share updates with all providers.

What’s Next for Medication Management
The field is evolving fast. AI-powered tools are coming that can scan all a patient’s prescriptions and flag dangerous interactions in seconds. By 2025, 65% of agencies are expected to use them. Some companies are adding QR codes to pill pouches. Scan the code, and a video plays in 17 languages showing how to take the pill. That’s huge for non-English speakers. But there’s a big challenge: staffing. The National Association for Home Care & Hospice reports a 28% vacancy rate for home health nurses. That means longer wait times and overworked staff. If you’re hiring privately, ask how many patients each nurse manages. If it’s more than 8-10 per day, that’s a red flag. The cost savings are real. Clarest’s economic study found medication management prevents about $1,200 in avoidable hospital costs per patient each month. That’s why Medicare is now tying reimbursement to adherence rates. Agencies that do it well get paid more. Those that don’t get penalized.Frequently Asked Questions
Can home health services give my loved one their pills?
Yes, but only if they’re licensed to do so. Medicare-certified home health agencies employ nurses or medication aides who are trained and authorized to administer medications. They follow strict protocols and never give pills unless it’s part of a doctor’s order. Unlicensed caregivers cannot give medications-they can only remind or assist.
Does Medicare cover home health medication management?
Medicare Part A covers medication management only if it’s part of a skilled care plan. That means the patient must be homebound and need skilled nursing services-like after a hospital stay, for wound care, or because of a new diagnosis. If someone just needs reminders, Medicare won’t pay. But if a nurse is needed to check for side effects, adjust doses, or coordinate with doctors, then yes-it’s covered.
What if my loved one takes herbal supplements or vitamins?
All supplements must be included in the medication list. Many seniors take fish oil, turmeric, or ginkgo biloba, thinking they’re harmless. But these can interact with blood thinners, blood pressure meds, and diabetes drugs. Home health nurses review every pill, capsule, and powder. They’ll flag any risks and suggest safer alternatives if needed.
How often should the medication list be updated?
The list should be reviewed every time there’s a change-new prescription, discontinued drug, or side effect. But at minimum, it should be fully updated every 30 days. Medicare requires agencies to reconcile medications during every care transition, like after a hospital visit or ER trip. Ask your provider how often they do full reviews.
What should I do if my loved one misses a dose?
Don’t double up. Call the home health nurse or prescribing doctor immediately. Some meds are safe to take late; others can be dangerous if taken too close to the next dose. The nurse will know the right action based on the specific drug. If you’re unsure, it’s always safer to skip than to risk an overdose.
Can home health services help with psychiatric medications?
They can assist with administration, but managing complex psychiatric regimens-like adjusting antidepressants or antipsychotics-is best handled by a psychiatrist or geriatric specialist. Home health nurses can monitor side effects, report changes in behavior, and ensure doses are taken on time. But dose changes should come from the prescribing doctor, not the home health team.



5 Comments
Hilary Miller-21 January 2026
My grandma uses this service and it’s been a game-changer-no more spilled pills or confusion at 2 a.m.
Sarvesh CK-22 January 2026
It's fascinating how systemic medication management transforms not just clinical outcomes but also the psychological burden on families. The mere act of reconciliation-verifying every pill, every supplement, every off-label use-creates a kind of narrative coherence in an otherwise fragmented healthcare journey. In India, where polypharmacy is rampant among elderly populations with multiple specialists, the absence of centralized documentation leads to catastrophic overlaps. I’ve seen a 78-year-old man on five antihypertensives because three different doctors assumed the others had it covered. Professional home health nurses don’t just administer-they synthesize. They become the central node in a network of disjointed care. And yes, the cost is a barrier, but the economic argument is irrefutable: one preventable hospitalization pays for six months of service. The real tragedy isn’t the lack of technology-it’s the lack of institutional will to integrate these services into standard geriatric protocols.
Keith Helm-24 January 2026
It is imperative to note that the term 'home health services' is often misapplied. Only Medicare-certified agencies employing licensed nurses may legally administer medications. Unlicensed caregivers who merely 'remind' patients are not qualified to handle pharmacological protocols, and permitting such practices constitutes a violation of federal regulatory standards.
Daphne Mallari - Tolentino-26 January 2026
How quaint. A plastic pill organizer? How very 2015. The real innovation lies in AI-driven pharmacovigilance platforms that cross-reference global drug interaction databases in real time-something no human nurse, no matter how diligent, can replicate. If you’re still relying on color-coded charts and teach-back methods, you’re essentially using a candle to light a nuclear reactor.
Neil Ellis-27 January 2026
This is the kind of quiet heroism we don’t celebrate enough. Picture a nurse showing up at 8 a.m., not with a clipboard full of jargon, but with a warm smile and a pouch labeled 'Morning Magic'-each pill a tiny act of love. No fanfare. No headlines. Just someone making sure an old man doesn’t choke on his own confusion. That’s not healthcare. That’s humanity with a stethoscope.