Understanding Hyperpigmentation in Skin of Color
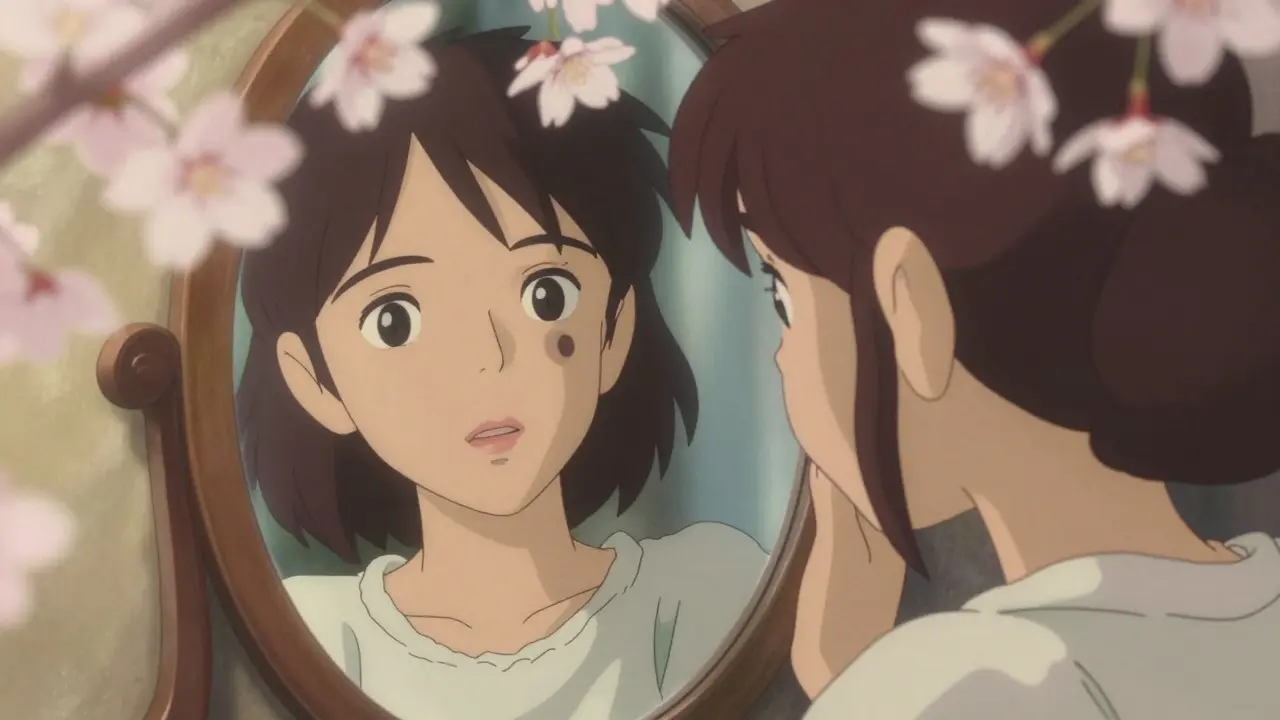
When discussing skin conditions in skin of color, hyperpigmentation is a common concern. It occurs when melanocytes produce excess melanin, leading to dark patches on the skin surface. This condition affects both men and women but is more prevalent in people with darker skin tones due to higher melanin content. According to the American Society for Dermatologic Surgery (ASDS), hyperpigmentation creates physical, emotional, and social challenges for patients.
Hyperpigmentation isn't just a cosmetic issue. It can manifest as light to dark brown or gray spots and patches. For those with skin of color, even minor skin trauma like acne or a cut can trigger noticeable dark spots. This makes managing hyperpigmentation especially important for maintaining skin health and confidence.
Common Causes of Hyperpigmentation
Several factors contribute to hyperpigmentation in skin of color. The most common is post-inflammatory hyperpigmentation (PIH), which occurs after skin injury or inflammation. Think of acne breakouts, eczema flare-ups, or even a minor scrape. These events cause inflammation, which then stimulates melanocytes to produce excess pigment.
Sun exposure is another major culprit. UV rays activate melanocytes, causing them to produce more melanin. This is why hyperpigmentation often gets worse with sun exposure. People with skin of color are particularly sensitive because their skin already has more melanin, which can be further stimulated by the sun.
Hormonal changes also play a role. melasma, a type of hyperpigmentation, appears as brown or gray patches on the face. It's more common in women, especially during pregnancy or when using hormonal contraceptives. Melasma is often referred to as the "mask of pregnancy" because it frequently occurs during this time.
How Hyperpigmentation Differs in Skin of Color
Hyperpigmentation looks and behaves differently in skin of color compared to lighter skin tones. On fair skin, hyperpigmentation might appear as faint freckles or sunspots. But in darker skin, it often shows up as more pronounced dark patches that can be harder to treat. This is because darker skin has more active melanocytes and higher baseline melanin levels.
Research from the PMC journal shows that facial hyperpigmentation is particularly distressing for people with skin of color. The condition can be more persistent and challenging to manage. For example, a simple acne breakout might leave a dark spot that lasts for months. This is why early treatment is crucial to prevent long-term discoloration.
Another key difference is how treatments work. Some procedures that help lighter skin tones might not be safe for darker skin. Chemical peels or laser treatments can sometimes cause more harm than good if not tailored to skin of color. This means treatment plans must be customized to avoid worsening the condition.

Treatment Options for Hyperpigmentation
Effective treatment starts with a solid skincare routine. Dermatologists often recommend a combination of topical creams and strict sun protection. Common ingredients include hydroquinone, which inhibits melanin production, and azelaic acid, which reduces inflammation and pigmentation.
Vitamin C is another popular choice. It's an antioxidant that brightens skin and protects against UV damage. Tretinoin, a retinoid, speeds up skin cell turnover, helping fade dark spots over time. For sensitive skin, kojic acid offers a gentler alternative.
Newer treatments are emerging too. tranexamic acid and cysteamine cream have shown promise in recent studies. These alternatives to hydroquinone are especially helpful for people who can't tolerate traditional treatments.
The Critical Role of Sun Protection
Sun protection isn't optional-it's non-negotiable for managing hyperpigmentation. UV rays worsen existing dark spots and can trigger new ones. Dermatologists stress that daily sunscreen use is the most important step in any treatment plan.
Choose a broad-spectrum sunscreen with SPF 30 or higher. Look for formulas with iron oxides, which block blue light from screens and devices that can darken skin. Tinted sunscreens work well for skin of color because they blend naturally and provide extra protection against visible light.
Apply sunscreen 15 minutes before going outside and reapply every two hours. Even on cloudy days, UV rays penetrate clouds and windows. Wear protective clothing like wide-brimmed hats and long sleeves when possible. These habits prevent further darkening and help existing treatments work better.

Addressing Underlying Causes
Treating the root cause of hyperpigmentation is essential. For example, if acne is triggering PIH, controlling breakouts will prevent new dark spots. Similarly, managing eczema or psoriasis can reduce inflammation-related pigmentation.
Review medications with your dermatologist. Some drugs, like certain antibiotics or antimalarials, can cause hyperpigmentation. If you're pregnant or using hormonal treatments, discuss this with your doctor. Hormonal changes often require specific skincare adjustments.
Regular check-ins with a dermatologist ensure your treatment plan stays on track. They can adjust prescriptions, recommend professional treatments, and monitor progress. Consistency is key-most patients see improvements after several months of dedicated care.
Recent Advances in Treatment
Dermatology research is constantly evolving. Recent studies highlight effective new treatments for hyperpigmentation in skin of color. Topical tranexamic acid has gained traction as a safe alternative to hydroquinone. It works by blocking the enzyme responsible for melanin production.
Cysteamine cream (5%) is another breakthrough. It's shown to reduce pigmentation without the side effects of traditional lightening agents. These innovations give patients more options tailored to their skin type.
Procedural treatments like laser therapy are improving too. Newer lasers target pigment more precisely, reducing risks for darker skin. However, these procedures should only be performed by dermatologists experienced in treating skin of color. Always discuss the pros and cons before trying new treatments.
Frequently Asked Questions
What causes hyperpigmentation in skin of color?
Hyperpigmentation in skin of color is often caused by inflammation from acne, eczema, or minor injuries. Sun exposure worsens it by stimulating melanin production. Hormonal changes, like during pregnancy, can also trigger melasma, a type of hyperpigmentation. Addressing the root cause is key to effective treatment.
How does sun exposure affect hyperpigmentation?
Sun exposure activates melanocytes, causing them to produce more pigment. This makes existing dark spots darker and can create new ones. People with skin of color are especially vulnerable because their skin has higher baseline melanin. Daily broad-spectrum sunscreen with iron oxides is essential to block UV and visible light.
What are the best topical treatments for hyperpigmentation?
Effective topical treatments include hydroquinone (2-4%), azelaic acid (15-20%), vitamin C serums, tretinoin, and kojic acid. Newer options like tranexamic acid and cysteamine cream are also effective. Always use these under a dermatologist's guidance to avoid irritation or side effects.
What is post-inflammatory hyperpigmentation (PIH)?
PIH is a type of hyperpigmentation that occurs after skin injury or inflammation. It's common in skin of color and can result from acne, cuts, burns, or even aggressive skincare. Unlike regular sunspots, PIH appears as dark patches where the skin was damaged. Treating the underlying inflammation is the first step to managing PIH.
What about keloids?
This article focuses on hyperpigmentation. Keloids are raised scars caused by excess collagen growth, which is a separate condition from hyperpigmentation. Current research on keloids in skin of color is limited, but treatments often involve corticosteroid injections, pressure therapy, or laser treatments. Consult a dermatologist for keloid-specific care.


Write a comment