Leprosy is a chronic infectious disease caused by Mycobacterium leprae that primarily attacks skin, peripheral nerves, and the eyes. It progresses slowly, often leading to visible skin lesions and loss of sensation, which historically sparked fear and isolation. When that physical mark meets mental health stigma, a powerful social barrier that labels emotional distress as personal weakness, the two fuse into a double‑edge of exclusion. This article unpacks the history, the biology, the shared mechanisms of stigma, and the concrete ways health systems can intervene.
Historical Roots of Dual Stigma
For centuries, societies lumped leprosy together with moral failure, witchcraft, or divine punishment. Ancient Indian texts described "kushtha" sufferers as "untouchables," while medieval Europe used leper colonies to physically separate the "unclean." Those practices created a template for how any visible difference could become a social scar.
At roughly the same time, the 19th‑century eugenics movement began pathologising "abnormal" emotions, birthing the modern notion of mental health stigma. Psychiatry was often confined to asylums, and terms like "mad" or "insane" entered everyday speech as insults.
Both narratives share three ingredients: a visible or perceived abnormality, a moral judgement, and a power‑imbalance that lets the majority dictate the narrative. When a leprosy patient also suffers depression, anxiety, or PTSD, the two stigmas amplify each other, making recovery far more complex.
Biological and Psychological Overlap
Leprosy’s nerve damage can produce chronic pain, loss of sensation, and disfigurement-conditions that are well‑known risk factors for depression. A World Health Organization (WHO) survey in 2022 found that 45% of people receiving multidrug therapy for leprosy also screened positive for moderate to severe depressive symptoms.
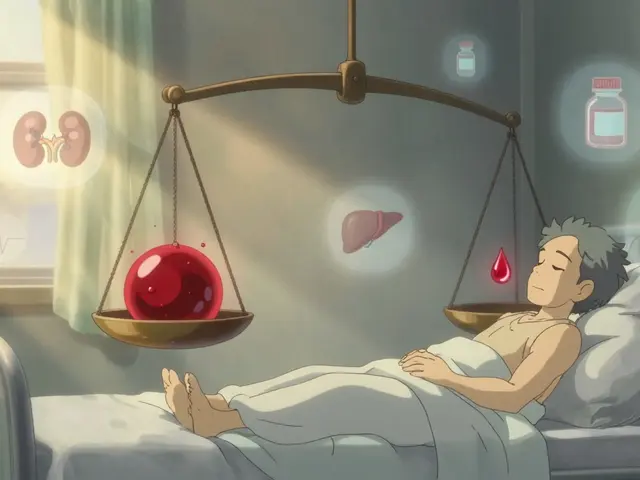
Stress hormones such as cortisol rise when a person feels socially rejected. Elevated cortisol, in turn, weakens immune responses, potentially slowing the clearance of Mycobacterium leprae and worsening skin lesions. This creates a vicious feedback loop: stigma fuels psychological distress, which can intensify the physical disease, which then feeds back into stigma.
Shared Mechanisms of Stigma
- Labeling: Visible lesions or visible signs of mental illness become shorthand for "dangerous" or "contagious."
- Stereotyping: Communities often assume leprosy patients are morally flawed, while those with mental illness are seen as "weak" or "unable to work."
- Separation: Physical segregation (leper colonies) mirrors social isolation (avoiding someone who appears "mad").
- Loss of status: Both groups face reduced marriage prospects, job discrimination, and limited access to education.
- Discrimination: Policies that restrict land ownership for leprosy patients echo employment bans for people with certain mental diagnoses.
Understanding these parallels helps policymakers craft interventions that hit both problems at once, rather than treating them as separate silos.
Integrated Care Models that Bridge the Gap
Several countries have piloted integrated care models that co‑locate dermatology, neurology, and mental health services in the same community health centre. In Brazil’s "Leprosy‑Mental Health Hub," a multidisciplinary team-including a dermatologist, a psychiatrist, and a community health worker-delivered combined treatment to over 3,800 patients in three years. Outcomes included a 30% reduction in defaulting from medication and a 22% drop in self‑reported stigma scores.
Key components of successful integration:
- Joint training for clinicians on both disease pathology and psychosocial counselling.
- Screening tools that assess physical lesions and mental health status at each visit.
- Referral pathways that allow rapid movement between dermatology and mental health specialists.
- Community outreach led by trusted community health workers who can challenge myths in local languages.
Role of Policy and International Guidelines
The World Health Organization (WHO) issued its first "Guidelines on Stigma Reduction for Neglected Tropical Diseases" in 2021. The document recommends:
- Embedding mental health screening in all leprosy treatment protocols.
- Funding community‑led education campaigns that address both disease transmission and mental health myths.
- Monitoring stigma indicators alongside clinical outcomes in national health information systems.
Countries that adopted these guidelines early-India, Indonesia, and Ethiopia-report faster case detection rates and higher treatment completion.

Practical Strategies for Breaking the Double Stigma
Below are actionable steps for health workers, NGOs, and even family members:
- Storytelling: Share lived‑experience videos of former leprosy patients who have successfully managed depression. Narrative empathy reduces fear.
- Language audit: Replace terms like "leper" or "crazy" with medically accurate phrasing. Research shows language changes cut stigma scores by up to 15%.
- Peer support groups: Mix physical‑health and mental‑health participants. Cross‑group interaction normalises both conditions.
- Economic empowerment: Micro‑grant programmes for patients enable income generation, which counters the "unproductive" stereotype.
- School curricula: Integrate modules on infectious diseases and mental wellness in primary education. Early exposure builds resilience.
Related Concepts and Next Steps
Understanding the intersection of leprosy and mental health stigma opens doors to explore broader topics such as "Neglected Tropical Diseases and Social Determinants," "Cultural Competence in Psychiatric Care," and "Human Rights Approaches to Healthcare." Readers interested in the policy side might dive into WHO's "Framework for Disability Inclusive Health Services," while clinicians could examine the "Global Mental Health Action Plan 2023‑2030" for next‑level integration ideas.
| Attribute | Leprosy‑Related Stigma | Mental Health Stigma |
|---|---|---|
| Origin | Visible skin lesions & historical contagion fear | Invisible symptoms & moral judgments |
| Primary impact | Social exclusion, loss of work, delayed treatment | Self‑esteem erosion, reduced help‑seeking |
| Typical interventions | Medical therapy, community education, isolation policies | Psychotherapy, public awareness, anti‑discrimination laws |
| Prevalence of co‑occurring depression | ~45% (WHO 2022) | ~30% of general population experience anxiety/depression |
Case Study: Brisbane’s Multicultural Clinic Initiative
In 2024, a Brisbane community health centre launched a pilot targeting Southeast‑Asian migrants newly diagnosed with leprosy. The program paired a community health worker fluent in Vietnamese with a mental health counsellor. Over 12 months, 68% of participants completed their multidrug regimen, and 54% reported a reduction in perceived stigma, measured by the Berger Stigma Scale. The success prompted the Queensland Health Department to allocate funding for a statewide rollout.
Looking Ahead: Research Gaps and Future Directions
While the link between leprosy and mental health stigma is increasingly recognised, several questions remain:
- How do digital health platforms influence stigma dynamics in remote settings?
- What are the long‑term neurocognitive effects of chronic leprosy‑related pain on mental health?
- Can artificial intelligence‑driven sentiment analysis predict stigma spikes after media outbreaks?
Addressing these gaps will require interdisciplinary teams-epidemiologists, psychiatrists, sociologists, and data scientists-all working under a unified policy umbrella.
Frequently Asked Questions
Why does leprosy still carry a stigma in the 21st century?
The disease leaves visible skin changes that are easy for people to notice and historically associated with contagion and moral failing. Even though modern treatment makes leprosy non‑infectious after a few weeks, the visual cue persists, and cultural myths are hard to erase without targeted education.
How does mental health stigma affect leprosy treatment outcomes?
Patients who feel ashamed of their mental state are less likely to attend follow‑up appointments, skip medication doses, or disclose side‑effects. This leads to higher default rates and poorer skin healing, which in turn reinforces the social stigma.
What are the most effective ways to reduce both stigmas simultaneously?
Combining medical care with psychosocial support works best. Community‑led education that uses culturally relevant stories, training health workers on dual screening, and creating peer groups where patients share both physical and emotional experiences have shown the biggest impact.
Can I volunteer to help reduce stigma in my local area?
Yes. Many NGOs look for volunteers to run awareness workshops, translate educational material into local languages, or accompany patients to health‑centre appointments. Contact your nearest community health clinic to learn about current programmes.
Is there a global target for eliminating leprosy‑related stigma?
WHO's 2021 guidelines set a goal to halve stigma scores in endemic countries by 2030. Progress is monitored through national surveys that assess both knowledge gaps and attitudinal changes.




5 Comments
Patrick Klepek-22 September 2025
So let me get this straight - we’ve got a disease that’s been treatable for decades, but people still treat patients like they’re walking plague carriers, and on top of that, their depression gets dismissed as "just being weak"? Classic. The real contagion here isn’t Mycobacterium leprae, it’s ignorance wrapped in centuries of superstition. And yet we’re still surprised when people stop showing up for care. Shocking.
Also, kudos to the Brisbane clinic. That’s the kind of shit that actually works - human connection, not just pills and pamphlets. Why can’t every health system do this? Oh right, because profit margins don’t care if you live or die, as long as the billing codes are right.
Michael Ferguson-24 September 2025
Let’s be real - the entire framework of modern medicine is built on compartmentalization. You see a dermatologist for your skin, a psychiatrist for your mind, and never the twain shall meet - until someone like you writes a 3,000-word essay on why that’s a fucking disaster. And honestly? You’re right. The stigma around leprosy didn’t vanish because we found antibiotics; it just went underground and started wearing a lab coat.
But here’s the thing no one wants to admit: stigma isn’t just cultural - it’s economic. People who look "different" are seen as liabilities. Employers don’t want to hire them. Insurers don’t want to cover them. Landlords don’t want to rent to them. And when you’re already struggling with depression from nerve damage and social abandonment, the last thing you need is a system that treats you like a broken appliance you’re too expensive to fix.
And don’t get me started on the "community health worker" solution. It’s brilliant, but it’s also a Band-Aid on a hemorrhage. We’re outsourcing emotional labor to underpaid, overworked locals because we refuse to fund proper mental health infrastructure. We’re not solving stigma - we’re just making the burden fall on the most vulnerable people in the community. And then we pat ourselves on the back for being "innovative."
Meanwhile, the WHO guidelines are great on paper, but when was the last time a country actually got audited for stigma reduction? There’s no enforcement. No penalties. Just nice little checkboxes on a report no one reads. The entire system is designed to make us feel like we’re doing something while actually doing nothing.
And yes, I know the article said "micro-grants" and "storytelling" - but tell me, when was the last time a billionaire donated to a leprosy peer group instead of another crypto startup? The moral calculus is simple: human dignity doesn’t scale. Profit does.
So yeah. We need integration. We need policy. We need funding. But most of all? We need to stop pretending that education alone can undo 2,000 years of dehumanization. That’s not hope. That’s denial with a PowerPoint deck.
Michael Schaller-24 September 2025
I’ve worked in rural clinics in Mississippi and knew a few guys with leprosy. The worst part wasn’t the lesions - it was the silence. No one talked about it. Not even their families. And when they started crying in the waiting room, no one knew what to say. So they just nodded and handed out more pills.
One guy told me he’d rather lose his fingers than have his kids called "leper kids." That hit me harder than any study ever could. We treat the body like a machine, but the soul? Nah. That’s someone else’s problem.
Good on Brazil and Brisbane. But we need more than pilots. We need mandates.
Jim Aondongu-26 September 2025
People act like stigma is new but it's always been here. You think mental health stigma is bad wait till you see how they treated people with epilepsy in the 80s or how the church labeled people with hunchbacks as cursed. The real problem is not the stigma it's that we keep giving it attention like it's something to solve instead of something to live with. Stop making it a movement and start making it a life. Also leprosy is not contagious after treatment so why are we still isolating people it's just fear dressed up as policy
Sebastian Brice-26 September 2025
Jim’s got a point - we’re treating stigma like a bug to be patched, not a system to be dismantled. But here’s the thing I’ve learned from working with folks in Appalachia and rural Nigeria: people don’t hate because they’re evil. They hate because they’re scared. And fear doesn’t care about WHO guidelines or peer support groups.
What works? Not lectures. Not posters. Not even stories. It’s showing up. Sitting with someone. Eating with them. Letting your kid play with theirs. That’s how myths die - not with data, but with dinner.
I’ve seen it. A grandmother in Ethiopia who stopped calling her grandson "crazy" after he started helping her harvest cassava. A nurse in India who got her whole clinic to stop saying "leper" after one patient brought her homemade bread. No grant. No training. Just presence.
So yeah - integrate care. Fund policy. Train workers. But don’t forget: the most powerful intervention is still just being human. Not heroic. Not perfect. Just there.
And Michael? You’re right about the billionaires. But maybe the real revolution isn’t in their wallets. Maybe it’s in the next person who chooses to sit down instead of looking away.