Every year, tens of thousands of people in the U.S. are harmed or die from medication errors - and most of them are preventable. The biggest culprit? Incomplete or inaccurate medical history. When you walk into a doctor’s office, emergency room, or hospital, the staff doesn’t know what you’re really taking unless you tell them - clearly, completely, and consistently.
It’s not just about remembering your prescriptions. It’s about the aspirin you take daily for heart health, the turmeric supplement your cousin swore by, the over-the-counter sleep aid you grab when you can’t shut off your brain at night. These all matter. And if they’re missing from your record, you’re at risk.
Why Your Medication List Is Your Lifeline
Medication reconciliation isn’t a buzzword. It’s a safety protocol required in every U.S. hospital and clinic since 2006. The goal? Make sure every medication you’re taking - and every one you’re not - is accounted for when you move between care settings. That means from home to ER, from hospital to rehab, from primary care to specialist.
Here’s the hard truth: when doctors rely only on what you remember, they miss about 25% of your medications. That number drops to 8% when they use electronic systems that pull data from pharmacies. But even those systems fail if you’re paying cash for meds, buying supplements online, or using a pharmacy that doesn’t share data.
Patients taking five or more medications - common among older adults and those with chronic conditions - are 88% more likely to have dangerous discrepancies. One wrong dose of blood thinner, one missed allergy, one unreported herb that thins your blood… and you could end up in the ICU.
What You Need to Track - Beyond Prescriptions
Most people think their medication list means pills from the pharmacy. It doesn’t. A complete list includes:
- All prescription drugs - even ones you stopped taking last month
- Over-the-counter meds - pain relievers, antacids, cold medicines, allergy pills
- Vitamins, minerals, and supplements - iron, magnesium, vitamin D, fish oil
- Herbal remedies - St. John’s wort, ginkgo, echinacea, garlic supplements
- Topical treatments - creams, patches, eye drops
- IV or injectable drugs - even if they were given at a clinic
Why does this matter? St. John’s wort can cancel out birth control. Garlic supplements can make blood thinners too strong. Ibuprofen can raise your blood pressure if you’re on ACE inhibitors. These aren’t rare interactions - they’re common, and they’re deadly if no one knows they’re happening.
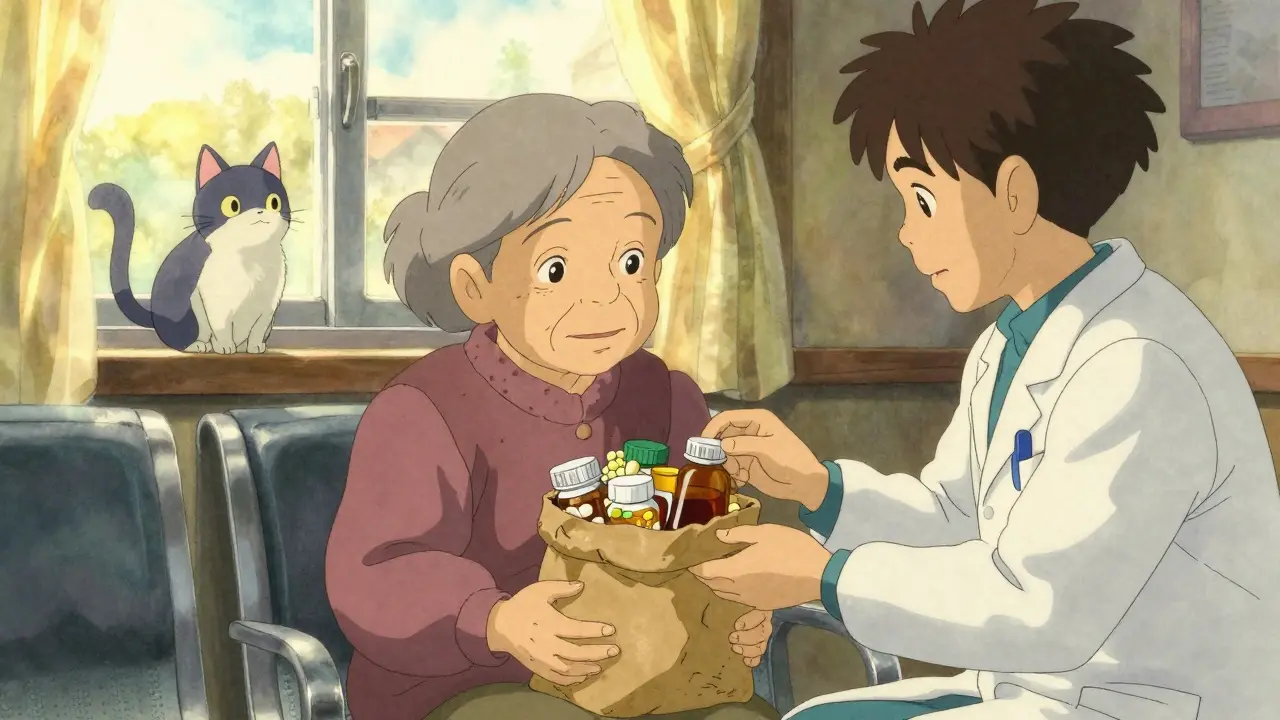
The Brown Bag Method: A Simple Fix That Works
There’s a reason nurses and pharmacists love the brown bag method. It’s old-school, but it’s the most reliable way to get the full picture.
Before your appointment, gather every pill bottle, capsule, patch, and liquid you take. Put them all in a brown paper bag - yes, literally. Bring it with you. No memory needed. No guessing. No “I think I take one of those every other day.”
Studies show this simple step reduces medication errors by 40%. Why? Because it forces accuracy. You can’t fake how many pills are left in the bottle. You can’t forget the gummy vitamins your grandkid gave you. You can’t say “I don’t take anything else” when the bottle of melatonin is right there.
Even better - take a photo of each bottle. Keep it on your phone. That way, if you forget the bag, you still have the visual record.

How Providers Use Your History - And Where It Falls Short
Hospitals now use electronic systems that pull your medication history from pharmacies. Surescripts, the biggest network, delivers over 3 billion medication records every year. That’s impressive. But here’s the catch: it only works if your pharmacy shares data - and not all do.
Online pharmacies? Cash-pay prescriptions? International meds? Those often don’t show up. Neither do most over-the-counter drugs. Only 33% of patients accurately report OTC use. And allergies? Half the time, they’re listed wrong or not at all.
Even with tech, systems still miss 48% of medication discrepancies. Why? Because computers can’t ask, “Are you still taking that herbal tea your aunt made you?” They can’t read between the lines of “I feel better now” or “I stopped because it made me dizzy.”
That’s why your voice matters more than ever. Technology helps. But you’re the only one who knows what you actually took - and why you stopped.
High-Risk Medications: Know the Red Flags
Some drugs are more dangerous than others - not because they’re bad, but because the margin for error is tiny. These are called “high-alert medications,” and they’re responsible for the most serious adverse events.
Examples:
- Insulin - too much can drop your blood sugar to life-threatening levels
- Warfarin and other blood thinners - too little risks clots; too much risks bleeding
- Intravenous oxytocin - used in labor, but a tiny dosing error can cause uterine rupture
- Chemotherapy drugs - narrow therapeutic window, high toxicity
- Antibiotics like vancomycin - kidney damage if levels aren’t monitored
If you’re on any of these, make sure your provider knows every other drug, supplement, or food you’re taking. For example, grapefruit juice can turn a common blood pressure pill into a dangerous overdose. That’s not a myth - it’s science.
What to Say - And How to Say It
Many patients freeze when asked, “What medications are you taking?” They say, “Oh, just the usual.” That’s not enough.
Use this simple structure:
- Situation: “I’m here for my annual checkup, and I want to make sure my meds are right.”
- Background: “I take lisinopril for blood pressure, metformin for diabetes, and aspirin daily. I also take omega-3s and a magnesium supplement.”
- Assessment: “I’ve been feeling more tired lately, and I think it might be the new sleep aid I started.”
- Recommendation: “Can we review if all of these are still safe together?”
This is called SBAR - a communication tool used by nurses and doctors worldwide. It’s not fancy. But it works. It cuts through confusion. And it saves lives.

What Happens When You Don’t Speak Up
One patient in Brisbane, 72, was admitted for pneumonia. She said she took “a few pills” - including her blood pressure med and a “vitamin.” She didn’t mention the blood thinner she’d been on for 10 years because she thought it was “just a supplement.”
Doctors gave her an antibiotic that interacted with the blood thinner. She bled internally. She spent 11 days in the hospital. Her recovery took months.
Another case: a 65-year-old man took melatonin every night. He didn’t tell his cardiologist. The doctor prescribed a new beta-blocker. The combination dropped his heart rate to 38 beats per minute. He passed out driving home.
These aren’t outliers. They’re routine.
Your Role in the System
You’re not just a patient. You’re a critical part of your own safety team. Providers can’t read your mind. Electronic records can’t fill in the gaps you don’t mention. Technology helps - but it doesn’t replace you.
Here’s what you can do today:
- Keep a written or digital list of every medication, updated after every visit
- Use the brown bag method at least once a year - or before any surgery or hospital stay
- Ask your pharmacist to print a current list - they have the most accurate record
- Check your patient portal. Is your list complete? If not, message your provider
- Bring a family member or friend to appointments if you’re on complex meds
- Speak up if something feels off - even if you’re not sure why
The system isn’t perfect. But you can make it work - if you show up with the full truth.
What’s Changing - And What’s Coming
By 2025, the U.S. government requires all hospitals to give patients direct access to their full medication history through secure portals. That’s a big step. But access doesn’t mean accuracy.
AI tools are being tested to predict interactions before they happen. Google Health’s prototype cut reconciliation time by 63% in trials. But AI can’t know you stopped taking your statin because it gave you muscle pain - unless you tell it.
Meanwhile, the FDA is pushing for clearer labeling on high-alert drugs. New rules will make insulin pens and blood thinners look less alike. That’s helpful. But again - it won’t fix what’s missing from your history.
The future of medication safety isn’t just better tech. It’s better communication. And that starts with you.
By 2030, experts estimate that if everyone shared their full medication history - accurately and consistently - we could prevent 1.2 million adverse drug events each year. That’s over 100,000 lives saved. And billions in healthcare costs avoided.
That future is possible. But only if you take the time to tell the truth - every time.




Write a comment