Insulin Temperature: What You Need to Know About Storage and Safety
When you use insulin, a life-saving hormone used to control blood sugar in people with diabetes. Also known as human insulin, it’s not just a pill you swallow—it’s a delicate biological product that can break down if not handled right. Many people think once insulin is in their fridge or pocket, it’s fine. But that’s not true. insulin temperature, the range of heat and cold insulin can safely be exposed to is critical. If it gets too hot—like left in a car on a summer day—or too cold—like frozen in the back of the fridge—it stops working. And you won’t always know until your blood sugar spikes for no reason.
Insulin is made of proteins. Proteins unravel when they’re too hot or frozen, and once that happens, they can’t do their job. The insulin storage, how insulin should be kept before and after opening rules are simple but easy to ignore. Unopened insulin goes in the fridge between 36°F and 46°F. Once you start using it, most types are good for 28 days at room temperature, up to 86°F. But if you’re in a place where it hits 90°F or higher—like a desert, a hot car, or a summer gym bag—that 28-day window shrinks fast. You might not see a change in color or smell, but your body will feel it.
People often confuse insulin spoilage, the process where insulin loses potency due to improper conditions with other issues like insulin resistance or pump malfunctions. But spoiled insulin is a silent problem. You might think your dose is too low, when really, the pen you’ve been using since March is just dead. That’s why checking the expiration date isn’t enough—you need to track how long it’s been out of the fridge and what kind of weather it’s seen. And if you ever drop your insulin, leave it in the sun, or think it might’ve frozen? Don’t risk it. Throw it out. It’s cheaper than a hospital visit.
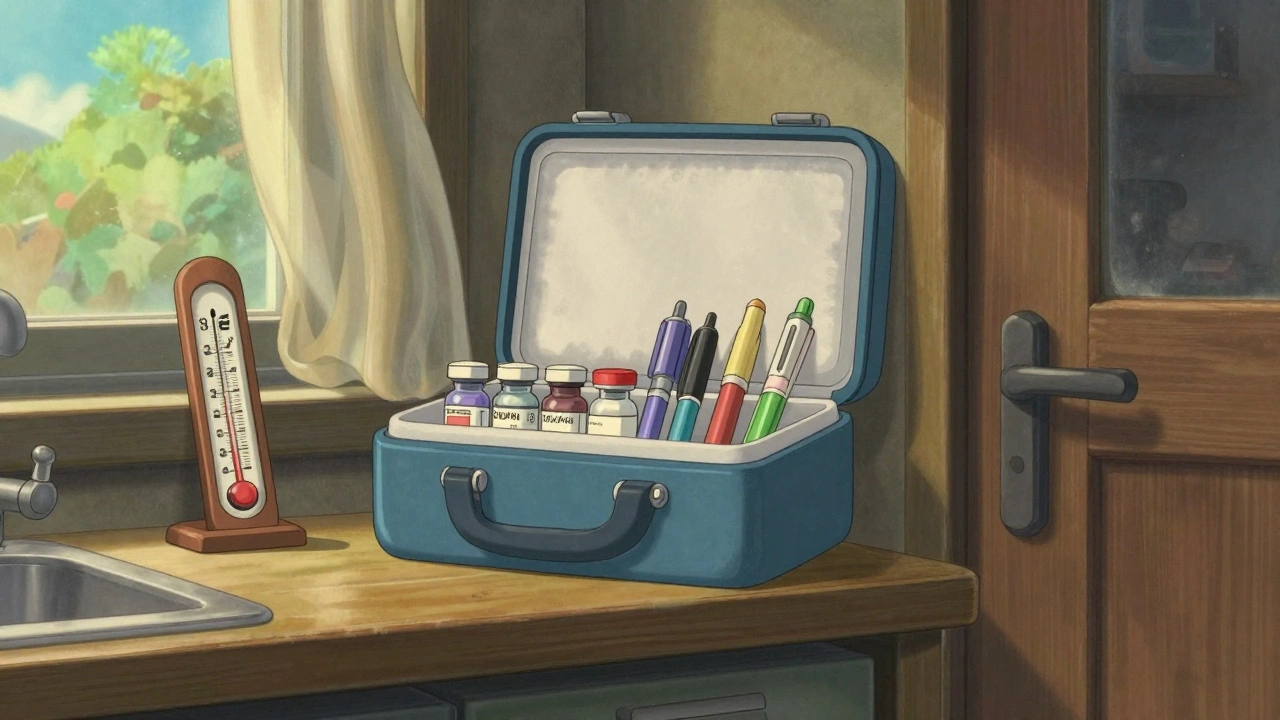
There’s no magic trick to keeping insulin stable, but there are smart habits. Use a small insulated bag with a cold pack when you’re out. Don’t leave it on the dashboard. Don’t store it in the bathroom where steam and heat rise. If you travel across time zones or fly, carry it with you—not in checked luggage. Airlines let you bring insulin on board, and TSA agents are trained to handle it. You don’t need a doctor’s note, but having one helps if you get questioned.
And what about insulin effectiveness, how well insulin works after being exposed to heat or cold? Studies show insulin exposed to temperatures above 86°F for more than a few days can lose up to 20% of its strength. That’s not a small drop. It’s enough to throw your blood sugar off track for days. If you’ve been feeling unusually tired, thirsty, or blurry-eyed and your doses haven’t changed, consider whether your insulin might be compromised.
Finally, insulin cooling, the methods used to keep insulin at safe temperatures during travel or extreme weather doesn’t need fancy gear. A simple insulated pouch with a reusable gel pack works. Some people even use a thermos with a little ice—just make sure the insulin doesn’t touch the ice directly. Freezing insulin permanently ruins it. If you see crystals or cloudiness where there shouldn’t be, toss it. No exceptions.
The posts below cover real cases, practical tips, and hidden dangers around insulin handling—from what to do when your power goes out, to how to tell if your insulin has gone bad without a lab test. These aren’t theoretical ideas. They’re lessons from people who’ve been there. You don’t need to guess. You just need to know what to look for—and what to do before it’s too late.
How to Store Insulin Pens, Vials, and Supplies Correctly
Learn how to properly store insulin pens, vials, and supplies to ensure they work effectively. Avoid common mistakes, understand temperature limits, and keep your diabetes management safe and reliable.