Kidney Function Dosing Calculator for Blood Thinners
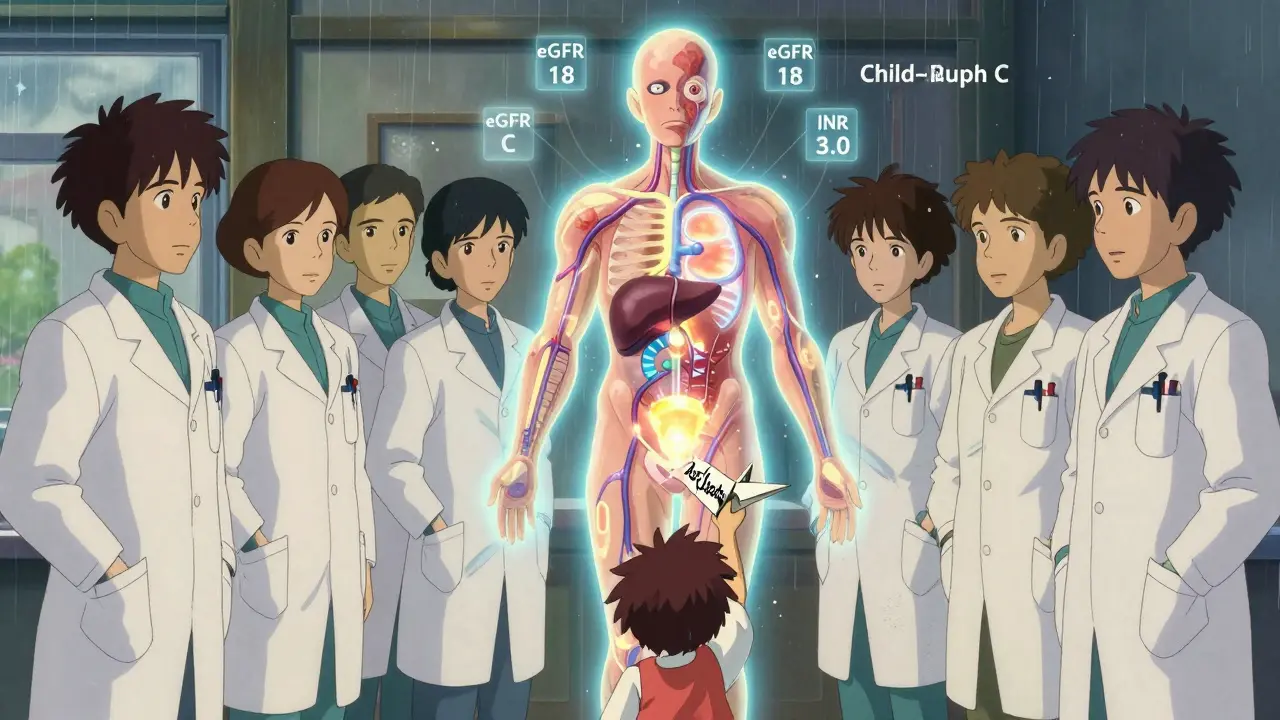
Calculate DOAC Dose Based on Kidney Function
Enter eGFR value to determine appropriate anticoagulant dose for kidney disease patients
Enter your eGFR to see recommended dose
Important Note: eGFR values may be inaccurate in advanced kidney disease. Always consult clinical guidelines before dosing.
Why Anticoagulation Gets So Complicated in Kidney and Liver Disease
When someone has both kidney disease and liver disease, taking a blood thinner isn’t like taking a daily pill for high blood pressure. It’s a tightrope walk between preventing clots and causing a deadly bleed. This isn’t theoretical - it’s happening every day in hospitals and clinics. About 1 in 4 people with atrial fibrillation also have chronic kidney disease, and nearly 1 in 7 have liver damage. Many of them need anticoagulation to avoid strokes, but standard guidelines don’t cover them. The drugs used for healthy people were never tested in these groups. That leaves doctors guessing.
How Kidney Disease Changes the Rules for Blood Thinners
Your kidneys don’t just filter waste - they clear most blood thinners from your body. When kidney function drops, those drugs build up. Too much? Bleeding risk skyrockets. Too little? Clots form. The problem? Standard tests like creatinine and eGFR can be wildly inaccurate in advanced kidney disease. One study found they’re off by 30-40% in people with stage 4 or 5 CKD. That means a patient might look like they have eGFR of 25 when they really have 18. Dosing based on that could be deadly.
Here’s what actually works in practice:
- Stage 1-3a (eGFR ≥45): All DOACs (apixaban, rivaroxaban, dabigatran, edoxaban) are fine at standard doses.
- Stage 3b (eGFR 30-44): Dose reductions kick in. Apixaban drops from 5 mg to 2.5 mg twice daily. Rivaroxaban from 20 mg to 15 mg daily. Edoxaban from 60 mg to 30 mg daily.
- Stage 4-5 (eGFR <30): This is where it gets messy. The EMA says no DOACs. The FDA says apixaban 2.5 mg twice daily is okay - based on a post-hoc analysis of the ARISTOTLE trial. That’s not the same as a real trial. But here’s the kicker: in this group, apixaban cut major bleeding by 70% compared to warfarin. No other DOAC has that kind of safety data.
- On dialysis: Rivaroxaban and dabigatran are risky. Dabigatran is 80% cleared by the kidneys - it piles up. Rivaroxaban’s levels are unpredictable. Apixaban? It’s the only one with real-world data showing it can be used at 2.5 mg twice daily. One nephrologist in Brisbane reported 15 dialysis patients on this dose for two years with zero bleeds. Another had a patient die from a retroperitoneal hemorrhage on the same dose. That’s the reality - no one knows for sure.
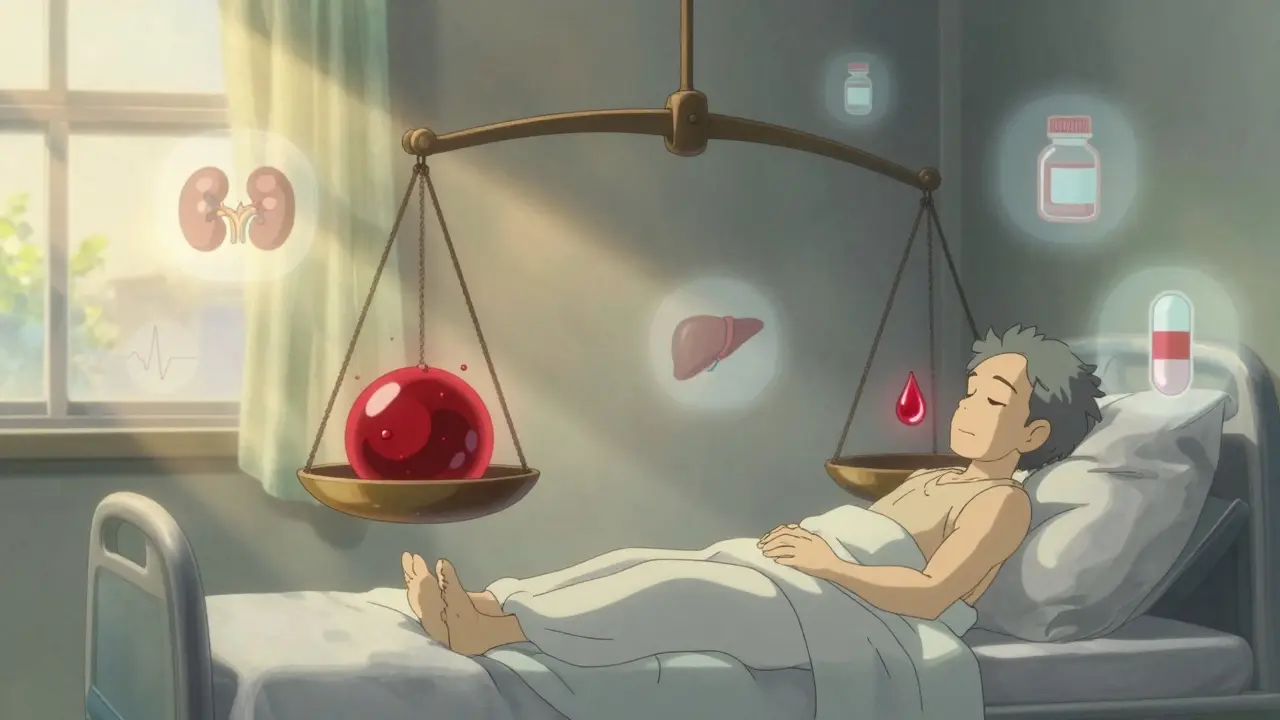
Warfarin? It’s still used in over 60% of dialysis patients. Why? Because we know how to reverse it. But INR targets get tricky. In eGFR under 30, many experts now aim for 1.8-2.5 instead of 2.0-3.0. Why? Because the blood is more fragile. Higher INR = higher bleeding risk. But lower INR = higher stroke risk. It’s a constant balancing act.
Liver Disease: When the Body Can’t Make Clotting Factors
The liver doesn’t just process drugs - it makes the proteins that help your blood clot. In cirrhosis, the liver can’t make enough of them. That means you’re both more likely to bleed AND more likely to clot. It’s a paradox. Platelet counts drop because the spleen swells and traps them. Over 75% of cirrhosis patients have platelets below 150,000. That’s not normal.
Child-Pugh score is the key. It’s a simple calculation based on bilirubin, albumin, INR, ascites, and mental status. It tells you how bad the liver damage is:
- Child-Pugh A (score 5-6): Mild disease. DOACs can be used at normal doses. Many hepatologists feel comfortable with apixaban or rivaroxaban here.
- Child-Pugh B (score 7-9): Moderate disease. Use DOACs with caution. Some reduce the dose. Others avoid them entirely.
- Child-Pugh C (score ≥10): Severe disease. DOACs are contraindicated. The RE-CIRRHOSIS study showed a 5.2-fold higher risk of major bleeding. That’s not a risk you take lightly.
Here’s the twist: INR doesn’t mean what you think it does in liver disease. INR only measures vitamin K-dependent factors. It ignores low platelets, low fibrinogen, high fibrinolysis. A patient with Child-Pugh C might have an INR of 1.5 - but still bleed like crazy. Or they might have an INR of 3.0 and never bleed. That’s why experts say: “Treat the patient, not the INR.”
Some centers use thromboelastography (TEG) or ROTEM to get a full picture of clotting. But only 38% of U.S. hospitals have these tools. In most places, doctors are flying blind.

DOACs vs. Warfarin: The Real Trade-Offs
Everyone wants to know: which is better? The answer? It depends on the organ damage.
In kidney disease, apixaban wins on safety. In the ARISTOTLE subgroup of patients with eGFR 25-30, apixaban cut major bleeding by 31% compared to warfarin. It also reduced intracranial hemorrhage by 62%. That’s huge. But in end-stage kidney disease - especially on dialysis - warfarin still has an edge because of reversal options. Andexanet alfa reverses apixaban and rivaroxaban, but it costs $19,000 per dose and isn’t available in most hospitals. Idarucizumab reverses dabigatran, but it’s useless for the others. Warfarin? You give vitamin K and fresh frozen plasma. It’s messy, but it’s everywhere.
In liver disease, warfarin’s big problem is unpredictability. In healthy people, INR stays stable. In cirrhosis, the variation is 42% higher. Only 45% of cirrhotic patients stay in the therapeutic range more than 60% of the time. That’s worse than flipping a coin. DOACs have more predictable levels - but if they build up, you can’t reverse them easily.
One study found that in cirrhotic patients with portal vein thrombosis, DOACs were actually safer than warfarin. Why? Because the clotting risk was so high, the bleeding risk was worth it. But for atrial fibrillation? The balance tips the other way. This isn’t one-size-fits-all. It’s case-by-case.
What Doctors Actually Do in Real Life
Here’s what happens in clinics, not just in guidelines:
- Only 28% of dialysis patients with atrial fibrillation get anticoagulation - even though 76% have a high stroke risk score (CHA2DS2-VASc ≥3). Fear wins over evidence.
- Of those who do get anticoagulation, 63% get warfarin. 37% get a DOAC - mostly apixaban.
- 18.7 bleeding events per 100 patient-years with warfarin. 14.2 with DOACs. But stroke rates? Nearly identical. That’s the trade-off.
- 41% of hepatologists adjust anticoagulation based on platelet function tests. 68% have had a major bleed in their cirrhotic patients in the last year.
- Reddit threads from nephrologists show the same tension: one doctor says apixaban 2.5 mg twice daily saved 15 patients. Another says it killed one. No one has the answer.
At Mayo Clinic, they require a joint nephrology-cardiology consult before starting anticoagulation in stage 4 or 5 CKD. At UCSF, they check platelets and MELD scores every month. Stop anticoagulation if platelets drop below 50,000 or MELD exceeds 20. These aren’t guidelines - they’re survival tactics.
What’s Coming Next
Two big studies are underway. The MYD88 trial is randomizing 500 dialysis patients to apixaban vs. warfarin. Results in 2025. The LIVER-DOAC registry is tracking 1,200 cirrhotic patients on DOACs worldwide. We’ll finally have real data.
The FDA is considering new labeling for apixaban in end-stage kidney disease. KDIGO is updating its guidelines in late 2024 with 17 new studies. That could change everything.
Right now, 1.2 million Americans with advanced kidney or liver disease are denied anticoagulation - not because they don’t need it, but because no one knows how to give it safely. That’s not just a medical gap. It’s a moral one.
What You Can Do Right Now
If you or someone you care about has kidney or liver disease and needs a blood thinner:
- Ask for the exact eGFR - not just “stage 3” or “advanced.” Get the number.
- Ask for the Child-Pugh score - if you have liver disease.
- Ask if your doctor has experience managing anticoagulation in this setting.
- Ask about apixaban - it’s the only DOAC with any real safety data in advanced disease.
- Ask about reversal options - what happens if you bleed? Can they stop it?
- Ask for a multidisciplinary consult - nephrologist, hepatologist, hematologist, cardiologist.
Don’t accept “we don’t know” as an answer. Say: “I need to know what you’re going to do - and why.”



4 Comments
Juan Reibelo-23 January 2026
This is one of those topics where guidelines are useless. I've seen patients on apixaban with eGFR 12 still getting 2.5mg twice daily because the lab said 'it's within range'-and then they bled out. The numbers lie. You have to look at the person, not the calculator.
Also, never trust a creatinine in someone with sarcopenia. Muscle mass matters more than the number on the screen.
Amelia Williams-25 January 2026
I love how this post cuts through the noise. So many docs just follow the algorithm like it’s a recipe. But real medicine? It’s messy. I’ve had patients with cirrhosis and CKD on rivaroxaban who were fine at 15mg because their INR stayed stable for 18 months. No guideline says that’s okay-but it worked. Trust your eyes, not just the eGFR.
Viola Li-27 January 2026
Honestly, why are we even using DOACs in these patients? They were never studied properly. Warfarin at least has a monitoring tool. This whole DOAC revolution feels like pharmaceutical marketing dressed up as science.
venkatesh karumanchi-27 January 2026
In India, we rarely have access to DOACs for advanced CKD patients. We use warfarin, adjust by INR, and pray. No fancy labs, no point-of-care eGFR recalculators. But we get by. Sometimes the simplest tools are the most honest.