Rescue Inhaler Selector
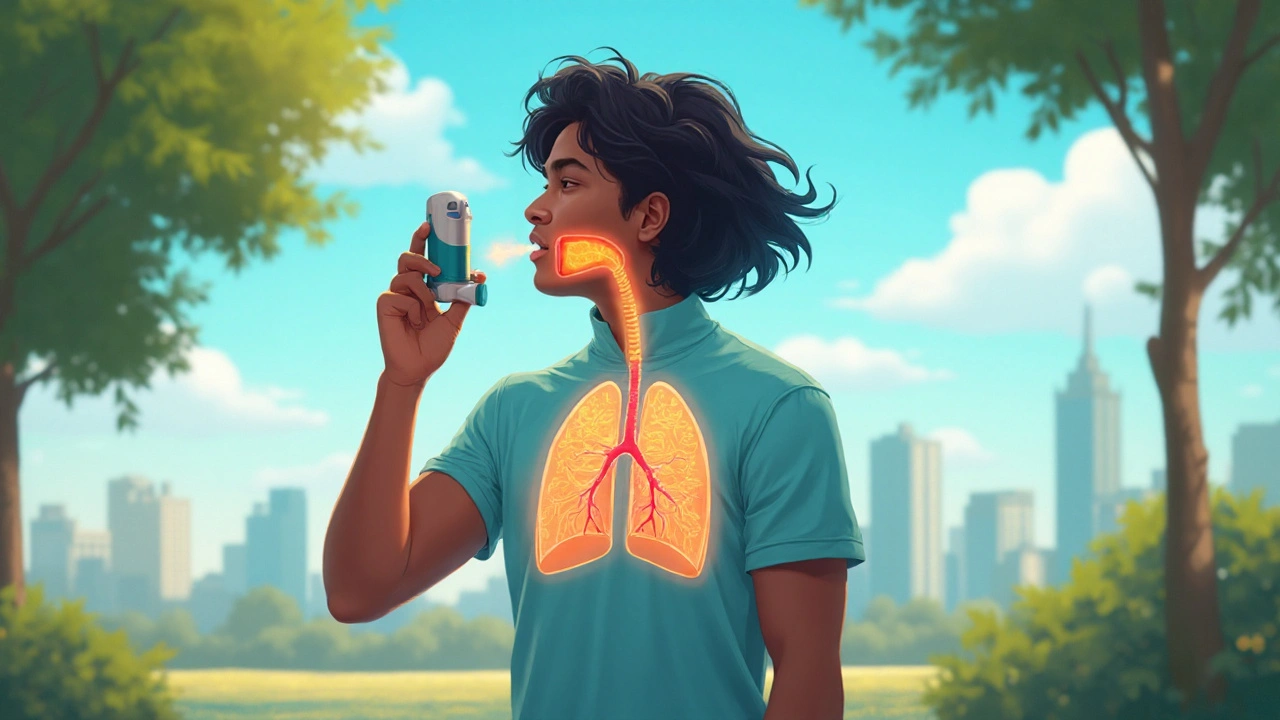
Asthalin is a brand‑name inhaler that contains salbutamol, a short‑acting beta‑2 agonist (SABA) used to quickly relax airway muscles during an asthma or COPD flare‑up. It delivers a rapid onset of relief, typically within 5‑10 minutes, and its effects last around 4‑6 hours. Asthalin is available in metered‑dose inhaler (MDI) and nebuliser formulations, making it a versatile rescue option for patients of all ages.
How Salbutamol Works
Salbutamol binds to beta‑2 receptors on bronchial smooth muscle, triggering a cascade that increases cyclic AMP and leads to muscle relaxation. The result is widened airways, improved airflow, and reduced wheezing. Because it acts directly on the receptors, the drug provides immediate symptom relief without altering the underlying inflammation.
Common Alternatives to Asthalin
When doctors talk about “rescue inhalers,” they often mention several other agents. Below are the most frequently prescribed alternatives, each with its own profile.
Ventolin is another brand of salbutamol, identical in active ingredient to Asthalis but marketed in different regions. Its formulation and dosing are equivalent, making it a direct substitute for patients who travel or change pharmacies.
Levalbuterol is the R‑enantiomer of albuterol (the US name for salbutamol). It offers a slightly lower risk of tremor and tachycardia while delivering comparable bronchodilation, positioning it as a “gentler” SABA for people sensitive to side effects.
Formoterol belongs to the long‑acting beta‑2 agonist (LABA) class. It provides a rapid onset (within 1‑3 minutes) *and* a prolonged duration of up to 12 hours, but because of its length it is only prescribed for maintenance, not acute rescue.
Salmeterol is another LABA with a slower onset (about 15‑30 minutes) but a 12‑hour effect. It must always be paired with an inhaled corticosteroid (ICS) for asthma due to safety guidelines.
Ipratropium bromide is an anticholinergic bronchodilator that works by blocking muscarinic receptors, reducing bronchoconstriction. It is slower (10‑15 minutes) and less potent than SABAs, but it is valuable in COPD and for patients who experience tachycardia with beta‑agonists.
Theophylline is an oral methylxanthine that relaxes airway smooth muscle and has anti‑inflammatory effects. Its onset is hours rather than minutes, and its therapeutic window is narrow, so it’s rarely first‑line today.
Side‑Effect Profiles
All bronchodilators share some core adverse effects-tremor, palpitations, and mild headache-but the intensity varies. SABAs like Asthalin often cause transient nervousness, especially at higher doses. Levalbuterol reduces these neurologic symptoms by about 30% in clinical trials. Anticholinergics such as ipratropium are more likely to dry the mouth but carry a lower cardiac risk. LABAs may increase the chance of asthma‑related paradoxical bronchospasm if used without an accompanying steroid.

Comparison Table
| Brand / Generic | Drug Class | Onset (min) | Duration (hrs) | Typical Dose (puffs) | Prescription Status | Typical Side‑Effects |
|---|---|---|---|---|---|---|
| Asthalin (Salbutamol) | SABA | 5‑10 | 4‑6 | 1‑2 puffs as needed | Rx (over‑the‑counter in some regions) | Tremor, tachycardia, headache |
| Ventolin (Salbutamol) | SABA | 5‑10 | 4‑6 | 1‑2 puffs | Rx/OTC | Same as Asthalin |
| Levalbuterol | SABA (R‑enantiomer) | 5‑10 | 4‑6 | 1‑2 puffs | Rx | Less tremor, similar cardiac effect |
| Formoterol | LABA | 1‑3 | 12 | 1‑2 puffs twice daily | Rx (must pair with ICS for asthma) | Potential tachycardia, rare paradoxical bronchospasm |
| Salmeterol | LABA | 15‑30 | 12 | 1‑2 puffs twice daily | Rx (must pair with ICS) | Headache, muscle cramps |
| Ipratropium bromide | Anticholinergic | 10‑15 | 4‑6 | 2 puffs four times daily | Rx | Dry mouth, cough |
| Theophylline | Methylxanthine | 60‑120 | 8‑12 | 150‑300mg oral BID | Rx | Nausea, arrhythmia (at high levels) |
Choosing the Right Rescue Inhaler
Think of rescue inhalers as a toolbox. You pick the tool that fits the job and the user’s tolerance. Here are the main decision points:
- Speed of relief: If you need relief within minutes, a SABA (Asthalin, Ventolin, Levalbuterol) is unbeatable.
- Duration: For occasional flare‑ups, a short‑acting agent is fine. For frequent night‑time symptoms, a rapid‑onset LABA like formoterol may be added to a maintenance plan.
- Side‑effect sensitivity: Patients with heart arrhythmias often prefer anticholinergics or levalbuterol.
- Cost and availability: Over‑the‑counter SABAs are cheaper in many countries, while LABAs require a prescription and a partner steroid.
- Device preference: Some users struggle with the hand‑breath coordination of MDIs. A spacer or a dry‑powder inhaler (DPI) can improve technique.
Practical Tips for Using Inhalers Effectively
Even the best drug fails if you can’t deliver it right. Follow these steps:
- Shake the MDI for 5 seconds.
- Exhale fully, then place the mouthpiece between your teeth and close your lips around it.
- Press down once while beginning a slow, steady inhalation.
- Continue inhaling for another 3‑4 seconds, then hold your breath for about 10 seconds.
- If a second puff is needed, wait 30 seconds before repeating.
Store inhalers at room temperature, away from direct sunlight. Replace the canister or device once the counter hits “0” or the dose‑counter indicates it’s empty.
Related Concepts and Next Steps
Understanding rescue inhalers fits into a larger picture of airway disease management. Two closely linked topics are asthma control, which focuses on daily inhaled corticosteroids, and COPD management, where long‑acting bronchodilators form the backbone of therapy. You’ll also encounter device categories like metered‑dose inhaler (MDI), a press‑urged canister that aerosolizes medication and dry‑powder inhaler (DPI), which relies on the patient’s inspiratory flow to disperse powder. Exploring these will help you match the right drug to the right device.
Future articles could cover:
- Step‑by‑step guide to choosing an appropriate inhaler device.
- How to create a personalized asthma action plan.
- Emerging biologic therapies for severe asthma.

Frequently Asked Questions
Is Asthalin the same as Ventolin?
Yes. Both contain the same active ingredient, salbutamol, and work identically. The difference is mainly branding and regional availability.
When should I use a LABA instead of a SABA?
LABAs are meant for long‑term control, not immediate relief. Use a LABA when you have frequent symptoms that persist beyond a couple of hours, but always pair it with an inhaled steroid for asthma.
Can I take levalbuterol if I get shaky after using Asthalin?
Levalbuterol often causes less tremor because it’s a single‑enantiomer formulation. Many patients switch to it after experiencing side‑effects with regular salbutamol.
Is ipratropium safe for children with asthma?
Ipratropium is approved for use in children over 6years for COPD‑like symptoms. For pure asthma, SABAs are preferred; ipratropium may be added in severe cases under specialist guidance.
Why does my inhaler feel empty before the dose count reaches zero?
A few factors can cause this: you might be inhaling too fast (wasting spray), the canister could be faulty, or the medication may have settled. Shake well, prime the inhaler, and if the problem persists, replace it.




20 Comments
Jay Crowley-25 September 2025
Asthalin delivers rapid bronchodilation within minutes.
sharon rider-29 September 2025
When you think of rescue inhalers, picture a toolbox rather than a single Swiss army knife. Each agent has its own strength, and the choice often reflects the patient’s lifestyle and side‑effect tolerance. Asthalin’s fast onset makes it a go‑to for sudden wheeze, while levalbuterol offers a gentler hand for the jittery. The key is matching the tool to the job, not just grabbing the cheapest option.
swapnil gedam- 4 October 2025
I agree, and I’d add that device preference can be just as crucial as the drug itself. Some patients struggle with the hand‑breath coordination of MDIs, so a spacer or a DPI can dramatically improve delivery. Also, watching for that “empty‑feeling” before the counter hits zero can save an asthma attack. It’s all part of personalising the toolbox.
Michael Vincenzi- 8 October 2025
Good point on spacers – I’ve seen kids get up to 50% more drug deposited when using one. Also, don’t forget to prime a new inhaler with a few sprays before the first dose. A quick shake and a slow, steady inhale are the secret weapons. Stay consistent, and the rescue will be reliable.
Courage Nguluvhe-13 October 2025
From a pharmacodynamic perspective, salbutamol’s β2‑adrenergic agonism triggers a rapid cAMP surge, leading to smooth‑muscle relaxation within seconds. The R‑enantiomer levalbuterol binds with similar affinity but exhibits reduced off‑target cardiac stimulation, which is why it’s labeled “gentler.” In contrast, ipratropium’s muscarinic blockade offers a slower yet sustained bronchodilation ideal for COPD phenotypes. Understanding these mechanisms helps clinicians tailor therapy beyond brand names.
Oliver Bishop-18 October 2025
In the US guidelines, Asthalin and its sister brands are classified as first‑line rescue agents, and insurance often lowers the out‑of‑pocket cost. If you’re traveling, just check the FDA‑approved equivalents to avoid prescription hurdles. The key is staying stocked – an empty canister is the worst enemy of an asthma action plan.
Alissa DeRouchie-22 October 2025
Wow, this whole “toolbox” metaphor is *so* overused! I mean, who even reads the fine print on those inhaler manuals? Just grab whatever looks shiny and hope for the best. And if it doesn’t work, blame the universe, not the drug.
Emma Howard-27 October 2025
Let’s keep it simple: shake, inhale, hold. Practice the 5‑second hold every time you use a puff – it maximises deposition. If you’re using a spacer, remember to wait a beat between puffs to let the aerosol settle. Consistency beats fancy tech any day.
dee gillette- 1 November 2025
While many praise the cost‑effectiveness of over‑the‑counter salbutamol, it’s worth noting that generic formulations sometimes vary in propellant quality, potentially affecting dose consistency. A clinician‑prescribed brand may provide more reliable dosing, especially for severe asthmatics.
Jasin P.- 5 November 2025
Oh great, another "quick fix" guide for asthma. As if inhalers are magic wands that solve everything. First, you actually need a proper diagnosis before you start playing with SABA and LABA. Then, there’s the whole issue of adherence – most patients forget to use their controller meds and rely solely on rescue inhalers. That’s why we see an uptick in ER visits despite the abundance of “fast‑acting” drugs. And let’s not forget the environmental impact of propellants; every puff adds to greenhouse gases. If you’re really concerned about your lungs, maybe focus on reducing triggers instead of obsessing over which brand you puff.
Lily Đàn bà-10 November 2025
Wow, such a dramatic rant – the irony is intoxicating. You’ve turned a simple rescue inhaler guide into a philosophy lecture. Still, you’re right: we need more than just a quick fix.
Joseph O'Sullivan-14 November 2025
Honestly, the whole “choose your tool” spiel feels like a sales pitch. Just give me a reliable inhaler and stop over‑complicating it with tables and jargon.
Conor McCandless-19 November 2025
Picture this: a patient standing at the crossroads of acute wheeze and chronic breathlessness, clutching a silver‑lined Asthalin inhaler in one hand, while the other hand trembles with the prospect of tachycardia. He peers into the shimmering horizon of pharmacology, where salbutamol promises a five‑minute reprieve, levalbuterol whispers a gentler sigh, and ipratropium offers a slower, steadier tide.
In the theater of the lungs, the bronchial smooth muscle contracts like a tightly wound string, and the β2‑agonists snap that string with a swift, almost theatrical flourish. Yet, the drama does not end there. The audience – the patient’s nervous system – may erupt into tremors, a chorus of palpitations, or a solo of dry mouth, each side‑effect a reminder that no hero is without flaw.
Meanwhile, the LABA protagonists, Formoterol and Salmeterol, parade onto the stage with promises of twelve‑hour endurance, but they demand a partnership with an inhaled corticosteroid, lest they betray the audience with paradoxical bronchospasm. The anticholinergic antagonist, Ipratropium, arrives from the shadows, offering a measured, less cardiac‑racing calm, yet takes longer to win the crowd’s applause.
Thus, the clinician, like a seasoned director, must choreograph the inhaler ensemble, balancing onset speed, duration, side‑effect profile, and the patient’s personal script. Only then does the performance culminate in a harmonious sigh of relief.
kat gee-24 November 2025
Nice poetic drama, but I just need a clear “use this, not that” list.
Iain Clarke-28 November 2025
For anyone unsure, a quick tip: always check the expiration date on your inhaler. An expired canister can deliver far less medication, rendering even the best drug ineffective.
McKenna Baldock- 3 December 2025
Just a note on terminology – the correct term is “β2‑agonist” rather than “beta‑2 agonist.” Consistency helps maintain professional standards.
Roger Wing- 8 December 2025
Did you know big pharma pushes SABAs to keep you dependent on their drugs? They hide the fact that over‑use can actually worsen airway inflammation.
Matt Cress-12 December 2025
Sure thing, the causaiton's all about packaging. Salbital is just a dipensary name making u think it's diffirent.
Andy Williams-17 December 2025
Correction: “causation” is spelled “causation,” and “different” is spelled correctly. Also, the brand is “salbutamol,” not “Salbital.”
Paige Crippen-21 December 2025
From a neutral standpoint, the data suggest that both Asthalin and Ventolin provide comparable relief when used as directed.