What Is Triple Inhaler Therapy for COPD?
Chronic Obstructive Pulmonary Disease (COPD) isn’t just about coughing and shortness of breath. For many people, it’s about flare-ups-sudden worsening episodes called exacerbations-that can land you in the hospital. Triple inhaler therapy combines three medications into one or two devices: a long-acting muscarinic antagonist (LAMA), a long-acting beta-agonist (LABA), and an inhaled corticosteroid (ICS). Together, they tackle airway narrowing, inflammation, and mucus buildup at the same time. This isn’t for everyone. It’s meant for those with moderate to severe COPD who keep having flare-ups-two or more moderate ones, or one severe one-in a year.
Before 2023, most patients started with just two drugs: a LAMA and LABA. But studies showed that adding an ICS helped certain people more. The key? Blood eosinophil levels. If your count is 300 cells/µL or higher, triple therapy can cut exacerbations by about 25%. If it’s below 100, you’re more likely to get pneumonia without any real benefit. That’s why doctors now test your blood before prescribing it.
Single vs. Multiple Inhalers: Which Works Better?
There are two ways to get triple therapy: one inhaler or three separate ones. Most patients end up on a single-inhaler device-like Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol) or Trimbow (budesonide/glycopyrronium/formoterol). These are easier to use. One puff, once a day. No juggling devices. Real-world data shows 78% of people stick with single-inhaler therapy after a year. For those using three separate inhalers, adherence drops to 62%. Why? People forget. They get confused. They don’t want to carry around three gadgets.
Switching from multiple inhalers to one device isn’t just convenient-it’s effective. A 2023 study found patients who made the switch had 37% fewer flare-ups in the next six months. The main reason? Simplicity. One inhaler means one routine. One less thing to mess up. And when you’re managing COPD on top of other health issues, that simplicity matters.
Who Benefits Most-and Who Doesn’t?
Not every COPD patient needs triple therapy. In fact, only about 15-20% of people with COPD meet the criteria. You’re a candidate if:
- You’ve had two or more moderate exacerbations in the past year
- Or one severe exacerbation that required hospitalization
- Your blood eosinophil count is 300 cells/µL or higher
If you don’t meet these, triple therapy won’t help-and might hurt. Studies show people with low eosinophils (<100 cells/µL) have a higher risk of pneumonia with ICS, and no reduction in flare-ups. Some even get worse. That’s why guidelines now stress precision: treat based on biology, not just diagnosis.
Even among those who qualify, not all triple inhalers are equal. Extrafine particle formulations like Trimbow (budesonide-based) penetrate deeper into the lungs and carry lower pneumonia risk than fluticasone-based ones like Trelegy. One 2021 study found fluticasone increased pneumonia risk by 83% compared to budesonide. That’s not a small difference. Your doctor should pick the right one for your profile.
The Real-World Problem: Cost and Access
Triple inhalers work-but they’re expensive. In the U.S., brand-name versions like Trelegy can cost $75-$150 a month out-of-pocket. Medicare beneficiaries report skipping doses because of cost. That’s not just inconvenient-it’s dangerous. Missing doses increases your risk of flare-ups, which leads to ER visits and hospital stays. And those cost far more than the inhaler.
Some clinics have started medication synchronization programs to help. Instead of refilling three different prescriptions at different times, you get them all at once. Others work with patient assistance programs to reduce costs. But access still varies wildly. In Europe, only 19% of eligible patients get triple therapy. In the U.S., it’s nearly 29%. Why? Reimbursement rules, formulary restrictions, and prescribing habits all play a role.
Why Some Experts Are Skeptical
There’s a heated debate in respiratory medicine. On one side, researchers like Professor Jadwiga Wedzicha say triple therapy delivers real, meaningful benefits for the right patients. The IMPACT and ETHOS trials showed clear reductions in exacerbations. But others, like Dr. John Blakey, argue those trials were flawed. Many participants were already on triple therapy before the study started. When they switched to dual therapy (LAMA/LABA) for comparison, they were suddenly pulled off their ICS-causing a spike in flare-ups. That made triple therapy look better than it really is.
Here’s the kicker: the FDA and EMA both rejected claims that triple therapy reduces death rates. No study has proven it saves lives. The benefit is about reducing hospital visits, not preventing death. And even that benefit fades over time. The biggest drop in exacerbations happens in the first 90 days. After that, the advantage shrinks. That’s why experts now say: start triple therapy, reassess in 3-6 months. If you’re not improving, you might not need it.
How to Know If It’s Working for You
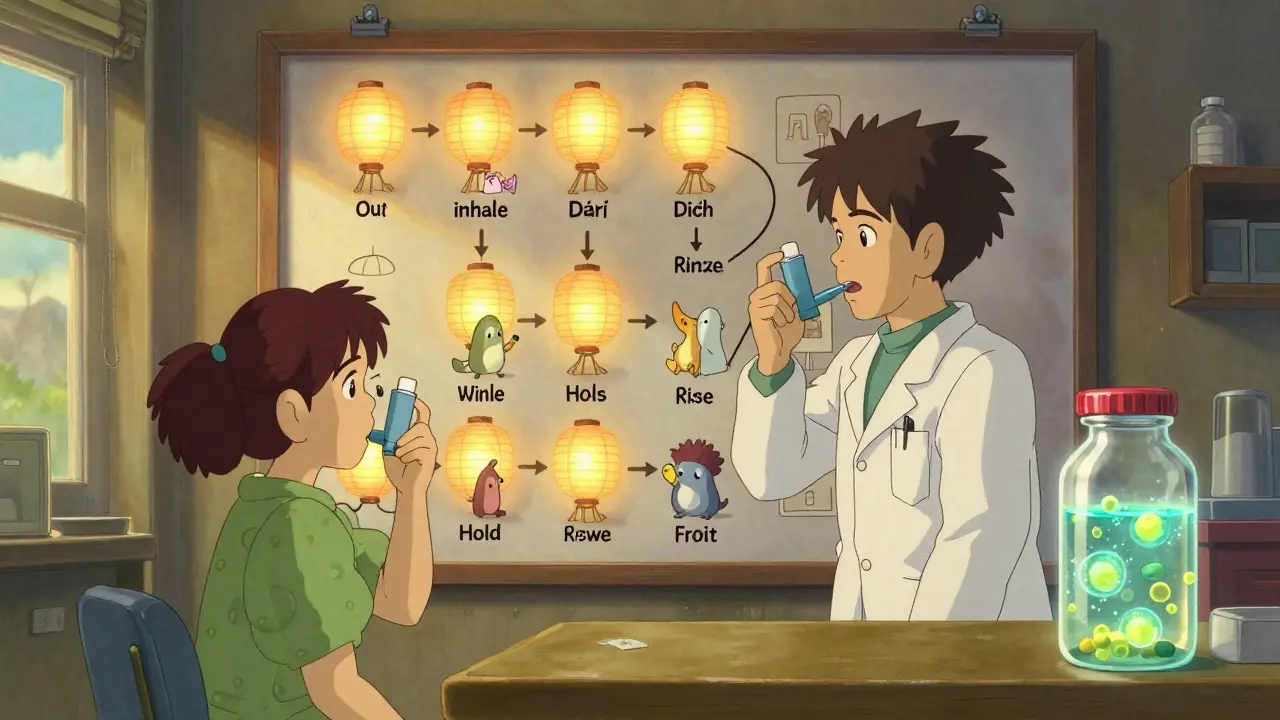
Just taking the inhaler isn’t enough. You have to use it right. Poor technique is the #1 reason people think their medication isn’t working. Studies show 50-70% of apparent treatment failures are actually just bad inhaler use. A simple checklist can fix that:
- Shake or load the device correctly
- Breathe out fully before inhaling
- Inhale slowly and deeply
- Hold your breath for 5-10 seconds
- Rinse your mouth after use (to prevent thrush)
Doctors should check your technique every visit. Many clinics now use video tools or digital inhalers that record your usage. If you’re still having flare-ups despite taking your meds, ask: Is it the drug? Or is it how I’m using it?
Also, monitor for pneumonia. Watch for fever, new or worsening cough, chest pain, or increased mucus. If you notice these, call your doctor. ICS increases pneumonia risk-especially with fluticasone. Quarterly spirometry tests help track lung function. If your FEV1 doesn’t improve after 3 months, your treatment plan may need a rethink.

What’s Next for COPD Treatment?
Triple inhalers are a step forward, but they’re not the endgame. Researchers are now testing whether other biomarkers-like fractional exhaled nitric oxide (FeNO)-can predict who responds better to ICS than eosinophils. Early results suggest FeNO might be more accurate. If proven, we could see even smarter prescribing by 2027.
Also on the horizon: biologics like dupilumab. Originally for asthma, it’s now being tested in COPD patients with high eosinophils. Early phase 3 data shows it reduces exacerbations even more than triple therapy in some cases. It’s an injection, not an inhaler. But for patients who keep flaring despite triple therapy, it could be the next step.
The future of COPD care isn’t about one-size-fits-all. It’s about matching the right drug to the right person. Blood tests. Inhaler checks. Regular follow-ups. And knowing when to stop something that’s not helping.
Key Takeaways
- Triple inhaler therapy (LAMA + LABA + ICS) reduces exacerbations only in patients with frequent flare-ups and blood eosinophils ≥300 cells/µL
- Single-inhaler devices improve adherence by 15-20% compared to multiple inhalers
- Fluticasone-based triple therapy carries higher pneumonia risk than budesonide-based options
- Cost is a major barrier-many patients skip doses due to price
- Poor inhaler technique causes most cases of apparent treatment failure
- Reassess triple therapy after 3-6 months; discontinue if no benefit
- Biologics like dupilumab may soon offer alternatives for high-eosinophil patients
Is triple inhaler therapy right for everyone with COPD?
No. Triple therapy is only recommended for people with moderate-to-severe COPD who’ve had two or more moderate exacerbations-or one severe one-in the past year, and who have blood eosinophil levels of 300 cells/µL or higher. For others, especially those with low eosinophils, it offers no benefit and increases pneumonia risk.
Can I switch from two inhalers to one triple inhaler?
Yes, and many patients benefit from the switch. Studies show better adherence and fewer flare-ups when moving from multiple inhalers to a single-device triple therapy. But this should be done under medical supervision. Your doctor will check your eosinophil levels and lung function before making the change.
Why do I need to rinse my mouth after using a triple inhaler?
The inhaled corticosteroid (ICS) in triple therapy can leave residue in your mouth and throat, increasing the risk of oral thrush (a fungal infection) and hoarseness. Rinsing with water and spitting it out after each use reduces this risk. Don’t swallow the rinse-just wash it out.
How long does it take for triple therapy to start working?
You may notice improved breathing within days, especially if you’ve been experiencing bronchospasm. But the full benefit-fewer flare-ups and better lung function-takes 3-6 months to show. Don’t stop the medication if you don’t feel better right away. Talk to your doctor before making any changes.
What are the signs that triple therapy isn’t working for me?
If you’re still having frequent coughing, wheezing, or flare-ups after 3-6 months, or if you develop new symptoms like fever, increased mucus, or chest tightness, your treatment may not be working. It could be poor inhaler technique, an incorrect diagnosis, or a need to switch medications. Your doctor may check your eosinophil levels again or consider alternatives like biologics.
Can I stop using my triple inhaler if I feel better?
Don’t stop without talking to your doctor. COPD is a chronic condition. Feeling better means the medication is working. Stopping suddenly can trigger a severe flare-up. Even if you’re stable, your doctor will likely recommend continuing therapy and reassessing every 6-12 months to see if you still need it.
What to Do Next
If you’re on triple therapy, make sure you’re using your inhaler correctly. Ask your doctor for a technique check. If you’re not on it yet but have frequent flare-ups, ask for a blood eosinophil test. If your count is high, discuss whether triple therapy could help. If cost is an issue, ask about patient assistance programs or generic alternatives. And always keep track of your symptoms-note when you feel worse, what triggers it, and how often you need rescue inhalers. That info helps your doctor decide if you’re on the right path.





8 Comments
Elen Pihlap- 8 January 2026
This made me cry. I’ve been on three inhalers for years and I still forget one every damn day. I just want to puff once and be done.
Ayodeji Williams- 9 January 2026
Bro, triple therapy is just Big Pharma’s way of selling you three pills in one fancy box. I’ve got COPD and I’m still breathing fine on just my LAMA. Why pay more? 😒
Emma Addison Thomas-10 January 2026
I’ve seen this play out in my NHS clinic-patients who switch to Trelegy report not just fewer flare-ups, but less anxiety about forgetting. It’s not magic, just better design. Simple is sustainable.
Anastasia Novak-11 January 2026
Let’s be real-this isn’t medicine, it’s a marketing masterpiece wrapped in eosinophil math. They took two proven drugs, threw in a steroid like it’s a free side of fries, and called it ‘revolutionary.’ The data? Solid for a subset. But let’s not pretend this isn’t a $1,200/month placebo with side effects. 🤡
And don’t get me started on how doctors skip the blood test and just prescribe it because ‘it’s easier.’ I’ve seen patients with eosinophils under 50 get triple therapy because their pulmonologist was in a hurry. That’s not care-that’s convenience.
Meanwhile, the real issue? Access. People in rural areas can’t even get the *single* inhaler, let alone the blood tests to justify it. So now we’re optimizing for the 15% who can afford it, while the 85% are left with expired inhalers and ER visits.
And yes, adherence improves with one device-but only if you can *afford* it. Insurance denies Trelegy all the time. So we’re praising convenience while ignoring equity. Classic.
Also, the pneumonia risk? Real. I had a friend on triple therapy who got pneumocystis pneumonia. She didn’t even have HIV. Just low eosinophils and a doctor who didn’t listen. So yes, the numbers look good. But medicine isn’t just stats. It’s people. And people aren’t data points.
Let’s stop calling this ‘breakthrough’ and start calling it ‘targeted escalation.’ And maybe, just maybe, fund home oxygen programs and pulmonary rehab instead of selling us glittery inhalers.
Aparna karwande-11 January 2026
India has over 40 million COPD patients and less than 5% have access to *any* inhaler, let alone triple therapy. You Americans talk about adherence like it’s a luxury, but here, we pray for a single nebulizer. This is not progress-it’s a Western fantasy. Stop exporting your pharmaceutical hype to developing nations. We need clean air, not fancy devices.
And don’t even get me started on how your ‘eosinophil cutoff’ ignores pollution-induced inflammation. Our patients have high eosinophils from diesel, not asthma. Your algorithm doesn’t work here. But your ads do. 🤬
Christine Joy Chicano-11 January 2026
Actually, the 2023 study on adherence and reduced exacerbations was peer-reviewed in The Lancet Respiratory Medicine-sample size over 12,000, longitudinal follow-up. The 37% reduction held even after adjusting for age, smoking history, and comorbidities. It’s not just ‘simplicity’-it’s pharmacokinetic synergy. The fixed-dose combo ensures consistent lung deposition.
And yes, eosinophils matter. But the cutoff isn’t arbitrary-it’s derived from post-hoc analyses of three major RCTs: ETHOS, KRONOS, and TRIMBO. The 300 cells/µL threshold has a 78% sensitivity for predicting exacerbation reduction. That’s not marketing. That’s evidence.
Also, the pneumonia risk is real but manageable: it’s ~1.5% higher over 12 months. Compare that to the 12-15% annual risk of hospitalization for frequent exacerbators. The math favors treatment for the right group.
And if you think this is ‘Big Pharma,’ tell that to the 78% of patients who report improved quality of life and fewer missed workdays. This isn’t a pill-it’s a lifeline.
Sai Ganesh-12 January 2026
In my clinic in Bangalore, we use generic LAMA/LABA combos and teach patients breath-holding techniques. No ICS. No Trelegy. Just education, clean stoves, and monthly check-ins. We’ve cut exacerbations by 40% in two years. Sometimes the simplest solutions-clean air, no smoking, breathing retraining-are more powerful than expensive inhalers.
Technology is useful, but not sacred. We must not confuse innovation with necessity.
Adam Gainski-12 January 2026
I’m a respiratory therapist and I’ve helped over 200 COPD patients switch to triple therapy. The biggest win? Not the stats-it’s the relief on their faces when they realize they don’t need to juggle four devices anymore. One puff in the morning. That’s it.
And yes, the eosinophil test is non-negotiable. I’ve seen too many patients get pneumonia because their doctor didn’t check. I always print the lab results and go over them with the patient. If it’s below 100? We stay on LAMA/LABA. No pressure. No upsell.
It’s not about the drug-it’s about the decision. And that decision should be informed, not automatic.
Also, if you’re on triple therapy and you’re still getting flare-ups? Check your inhaler technique. 60% of patients use it wrong. A simple demo with a spacer can change everything.
This isn’t a magic bullet. But for the right person? It’s the best thing that’s happened to their lungs in years.