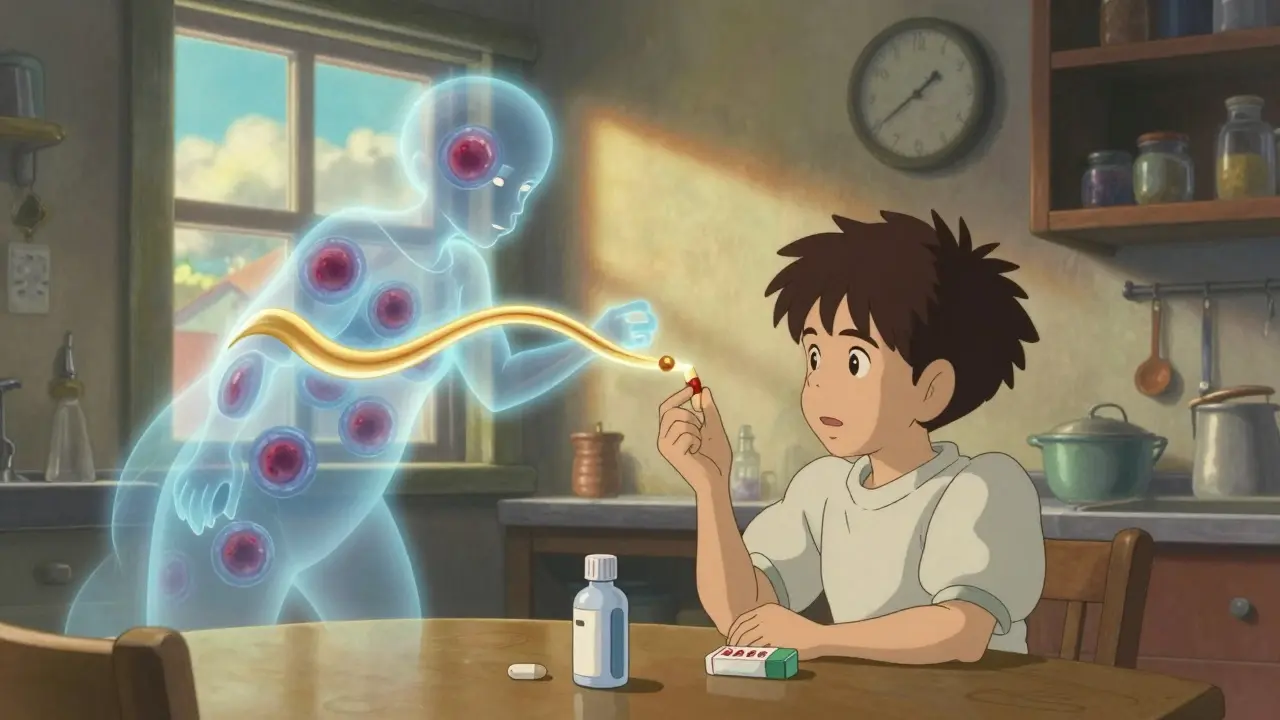
When you pick up a prescription, you might see two options: the familiar brand-name drug with a big logo, or a plain white pill with a code printed on it. The generic version costs a fraction of the price. But is it the same? This isn’t just about saving money-it’s about whether your treatment still works the way it should.
They’re Not Just Cheaper Copies
Generic drugs aren’t knockoffs. They’re exact copies of the active ingredient in brand-name medicines. If your doctor prescribes Lipitor (atorvastatin), the generic version has the exact same chemical compound: atorvastatin calcium. Same strength. Same pill shape. Same way it’s swallowed or injected. The FDA requires this. No exceptions.
The difference? The inactive ingredients. Things like dyes, fillers, and coatings. These don’t affect how the drug works in your body. But they can change how the pill looks or tastes. That’s why a generic version of your pill might be a different color or have a different shape. It doesn’t mean it’s weaker.
How Do We Know Generics Work the Same?
The FDA doesn’t ask generic manufacturers to run new clinical trials on thousands of patients. That would be expensive and unnecessary. Instead, they require a test called bioequivalence.
Here’s how it works: 24 to 36 healthy volunteers take both the brand-name drug and the generic version, in random order, with a break in between. Blood samples are taken over time to measure how much of the drug gets into the bloodstream and how fast. Two key numbers are checked: the peak concentration (Cmax) and the total exposure over time (AUC).
The generic must deliver the drug within 80% to 125% of the brand-name drug’s levels. That’s not a 20% difference in strength-it’s a statistical range that accounts for normal variation in how people absorb medicine. In real-world studies, the average difference in absorption between generics and brand names is just 3.5%. That’s less than the natural variation you’d see if you took the same brand-name pill twice on different days.
Since 1996, over 2,000 bioequivalence studies have been done. In 98% of them, the generic’s AUC was within 10% of the brand. That’s not close-it’s nearly identical.
Cost Savings Are Real-And Massive
Brand-name drugs cost 80% to 85% more than generics. On average, a 30-day supply of Lipitor costs $335. The generic? $0.00 with a coupon. Plavix? $450 brand, $0 generic. These aren’t outliers. This happens across the board.
In 2023, generic drugs saved the U.S. healthcare system $373 billion. That’s not a small number. That’s enough to cover the annual cost of treating every person with diabetes in the country-twice over.
Even when you pay out of pocket, the savings are clear. A generic statin might cost $4. A brand-name one? $150. That’s not a choice-it’s a necessity for people on fixed incomes.
But Not All Drugs Are Created Equal
There’s one big exception: drugs with a narrow therapeutic index (NTI). These are medicines where even a tiny change in blood levels can cause serious problems-either the drug stops working or it becomes toxic.
Examples: warfarin (blood thinner), levothyroxine (thyroid hormone), phenytoin (seizure control), and lithium (bipolar disorder). For these, small differences in absorption matter more.
That doesn’t mean generics are unsafe. It means you need to be careful when switching. If you’ve been stable on a brand-name version of warfarin for years, switching to a generic might require a blood test a week or two later to check your INR levels. Same with levothyroxine-some patients report feeling different after switching, even though studies show no overall difference in outcomes.
The FDA rates generics with an AB system. AB-rated means proven bioequivalent. B-rated means the generic meets FDA standards but may have slightly different absorption. For NTI drugs, pharmacists are often required to get your doctor’s approval before switching.
What the Evidence Says: Real Patients, Real Results
A 2020 study in Scientific Reports followed 1.2 million patients across 17 drug classes. It found that for 10 of the 17 drugs, generics were linked to fewer deaths. For 11, they were linked to fewer heart attacks and strokes. The generics didn’t just match the brand names-they outperformed them in some cases.
Another study of 38 cardiovascular trials found clinical equivalence in 35 of them. That includes statins, beta-blockers, ACE inhibitors, and even warfarin. The few exceptions weren’t because generics were weaker-they were because of how the studies were designed.
Yet, many people still don’t trust them. A 2022 survey found 43% of patients believed generics were less effective. One in four refused to take them when offered. Why? Fear. Misinformation. Marketing.
Brand-name companies spend billions on ads that make you think their version is superior. They don’t say it outright. But they hint at it. "The original. The trusted choice." Meanwhile, the generic sits quietly on the shelf.

What Pharmacists and Doctors Know
Most doctors and pharmacists know the science. A 2023 survey of 512 physicians found 78% correctly identified warfarin as a drug needing monitoring after a switch. But only 32% knew levothyroxine was in the same category. That’s a gap.
Pharmacists use the FDA’s Orange Book to find which generics are rated AB. That’s the gold standard. If your prescription says "dispense as written," that means your doctor wants you to stay on the brand. But if it’s not marked, the pharmacist can legally substitute a generic.
For most drugs-antibiotics, blood pressure pills, antidepressants, cholesterol meds-substitution is safe. No monitoring needed. No extra tests. Just the same effect, at a tenth of the price.
What You Should Do
Ask your pharmacist: "Is this generic AB-rated?" If yes, you’re good to go.
If you’re on warfarin, levothyroxine, phenytoin, or lithium, ask your doctor if switching is safe. Get a blood test 7 to 14 days after the switch.
Don’t assume the brand is better. The data doesn’t support it. The cost difference is too large to ignore.
And if you’ve had a bad experience with a generic-like feeling worse after switching-it’s worth reporting to your doctor. It might not be the drug. It could be the filler. Some people are sensitive to dyes or lactose. But that’s rare. And it’s fixable.
What’s Coming Next
The FDA is speeding up approvals for complex generics-things like inhalers, creams, and injectables-that used to take years to match. In 2023, they approved 247 of them, up 19% from the year before.
Biosimilars, which are generic versions of biologic drugs (like Humira or Enbrel), are starting to appear. They’re not exact copies, but they’re close enough to save 15% to 30%. That’s the next wave of cost savings.
And research is getting better. A 2023 MIT study showed new tech can now measure drug absorption so precisely that the variation between brand and generic for warfarin is falling below 2%. That’s better than most people realize.
Still, supply chain issues remain. In 2023, there were 312 shortages of generic drugs-mostly sterile injectables. That’s up 17% from 2022. It’s not about quality. It’s about manufacturing and raw materials. But that’s a separate problem.
Bottom line: For 90% of prescriptions, generic drugs are just as safe and effective as brand names. They’ve been proven by millions of patients, thousands of studies, and decades of real-world use.
The only reason to stick with the brand? If your doctor specifically tells you to. Otherwise, take the generic. Save the money. And know you’re getting the same medicine.




14 Comments
Christina Widodo-14 January 2026
I used to be super skeptical about generics until my insurance forced me to switch from Brand-X statin to the generic. I was convinced I’d feel awful-but nada. Same energy, same lab results. Even my cardiologist was surprised. Now I ask for generics first. Save $150 a month? Hell yes.
Also, the dye thing? Real. My generic pill had red dye and I got a weird rash. Switched to a different generic with no dye-problem solved. Not the drug, just the filler. Weird, but true.
Prachi Chauhan-14 January 2026
Why do we still think medicine is magic? It’s chemistry. Same molecule. Same action. Same result. The brand just has a better ad agency. We worship logos like they’re gods. But the pill doesn’t care if it’s labeled ‘Lipitor’ or ‘atorvastatin’. It just does its job. The real drug is the compound-not the marketing.
Stop paying for packaging. The body doesn’t read the box.
Katherine Carlock-16 January 2026
This is such a needed conversation. I’ve had family members refuse generics because they ‘feel different’-but when we dug into it, they’d switched from one generic to another, not brand to generic. The color changed. The shape changed. They thought the medicine changed. It’s psychology, not pharmacology.
Also, shoutout to pharmacists who actually explain this stuff. Too many just hand over the pill and walk away. We need more of them.
Sona Chandra-17 January 2026
OMG I CAN’T BELIEVE PEOPLE STILL BUY BRANDS. YOU’RE GETTING SCAMMED. I SAW A GUY PAY $140 FOR A BRANDED ANTIBIOTIC WHILE THE GENERIC WAS $3. HE SAID ‘BUT IT’S THE ORIGINAL!’ I ALMOST CRIED. WHO’S PAYING FOR YOUR MEDS? YOUR GRANDMA’S PENSION?!
Rinky Tandon-18 January 2026
Let me break this down for the clueless: bioequivalence is a statistical loophole. 80–125%? That’s a 45% window. You’re telling me a drug that’s 20% less potent is ‘the same’? And you call that science? No. That’s corporate compromise disguised as regulation.
And don’t get me started on the ‘98% success rate’-that’s cherry-picked data. What about the 2% who had strokes? Were they just unlucky? Or were their generics under-absorbed?
And who’s monitoring the 312 shortages? The same companies that own the patents? Yeah, right.
Rebekah Cobbson-19 January 2026
Thank you for writing this with so much clarity. I’ve seen too many people afraid to switch because of fear, not facts.
One thing I’d add: if you’re on levothyroxine and feel off after switching, don’t assume it’s ‘all in your head.’ Request a TSH test. It’s quick, cheap, and it’ll tell you if your dose needs adjusting. Most doctors don’t mention this, but it’s critical.
And if your pharmacist says ‘this one’s AB-rated’-believe them. They’re the real heroes here.
Alice Elanora Shepherd-21 January 2026
Excellent, comprehensive breakdown-thank you. I’d only add: the FDA’s AB rating system is robust, but it’s not perfect. Some generics, especially for NTI drugs, may vary slightly in dissolution rate due to manufacturing differences, even if they meet bioequivalence thresholds.
That said, for 90% of prescriptions, the data is overwhelming: generics are safe, effective, and cost-saving. The real issue isn’t the science-it’s the fear-mongering by pharma marketing departments.
Also: if you’re on warfarin, ALWAYS check your INR after switching. It’s not about trust-it’s about safety.
jordan shiyangeni-22 January 2026
Let’s be clear: this whole ‘generics are fine’ narrative is a dangerous myth perpetuated by bureaucrats and corporate cronies who don’t care about patient outcomes. You think a pill made in a factory in India with 30% cheaper labor is equivalent to one made in a GMP-certified U.S. facility? Please. The inactive ingredients alone can alter absorption kinetics in ways that aren’t captured by Cmax and AUC metrics-especially in elderly patients with altered GI motility.
And let’s not forget: the 2020 study you cited? It was funded by the Generic Pharmaceutical Association. Surprise, surprise. Where’s the independent, long-term, multi-center trial? Oh right-there isn’t one. Because the industry doesn’t want to fund it. They’ve already won the PR battle. But don’t fool yourself-your body isn’t a lab rat in a 24-person bioequivalence study.
And for the record: if you’re taking a generic for your heart medication, you’re gambling. Not with money-with your life.
Eileen Reilly-23 January 2026
ok so i switched my generic zoloft to the brand bc i felt ‘off’ and then i realized i just forgot to take it for 3 days and my anxiety spiked and i blamed the pill lmao
also my aunt took a generic blood pressure med and said it made her ‘tired’ so she switched back and now she’s fine… but she also drinks 6 energy drinks a day so idk what’s even real anymore
generic = cheaper. brand = expensive. both work. stop making it a thing.
Cecelia Alta-24 January 2026
Look, I get it. You want to save money. But let’s be real-your ‘generic’ statin was made in a factory that got fined for falsifying data last year. And the ‘bioequivalence’ study? 24 healthy 22-year-olds? What about people with kidney disease? Diabetes? GERD? You think the same absorption curve applies?
And why is it that when a generic fails, it’s ‘patient noncompliance’? But when a brand fails? Oh, it’s ‘rare side effect.’
Also, why are we still using dyes? Who thought that was a good idea? I don’t want my pills to look like candy. And don’t even get me started on lactose fillers. You think everyone can digest that? No. But no one cares. Because profit.
And yeah, I know the stats. I’ve read the studies. But I’ve also seen people crash after switching. And no one listens. Because ‘it’s just a pill.’
steve ker-25 January 2026
Generics are for poor people. Brand name is for those who know quality. Why do you think rich people don’t take generics? Because they know better. The science is a lie. The system is rigged. But the truth? You get what you pay for.
And stop pretending this is about health. It’s about control. Corporations want you to be cheap. They don’t care if you live or die. They just want your money. So take the expensive pill. Be the exception. Be the one who doesn’t fall for the scam.
George Bridges-26 January 2026
As someone who grew up in Nigeria and now lives in the U.S., I’ve seen both systems. In Lagos, generics are all we have-and they save lives. Here, people treat them like they’re dangerous. It’s not about the drug. It’s about privilege.
I’ve watched my cousin in Lagos take a generic antiretroviral for 12 years. Alive. Healthy. Working. No hospitalizations. Meanwhile, my cousin in Ohio refuses generics because ‘they’re not the real thing.’
Same molecule. Same effect. Different mindset.
Stop equating cost with quality. It’s not the pill that’s cheap. It’s the fear.
Audu ikhlas-26 January 2026
Who even cares about your FDA studies? In Nigeria we know real medicine. Your generics are made from scraps. Your regulators are bought. Your doctors are brainwashed. I took a generic for malaria once. Almost died. Now I only take the brand. Because I’m not a lab rat for American capitalism.
And don’t tell me about cost. I’d rather pay $1000 than die because some Indian factory cut corners. Your science is weak. Your trust is broken. Your system is corrupt.
Sonal Guha-28 January 2026
Generic = bad. Always. I don’t care what the data says. My friend’s mom had a stroke after switching. Coincidence? Maybe. But I’m not taking chances. Why risk it? Just pay the extra $140. Your life is worth more than a coffee.