When your hip starts to ache with every step, it’s not just discomfort-it’s your body screaming that something’s wrong. Osteoarthritis of the hip isn’t just wear and tear. It’s cartilage breaking down, bone grinding on bone, inflammation flaring up, and your ability to move slipping away. And if you’re carrying extra weight, you’re not just living with pain-you’re accelerating the damage.
For years, doctors told people with hip osteoarthritis to lose weight. But lately, some experts have questioned whether it even helps. One 2023 commentary in NEJM Journal Watch bluntly stated, “Osteoarthritis of the Hips Is Unaffected by Weight Loss.” That sounds like bad news. But here’s what they didn’t say: the latest science tells a very different story.
Weight Loss Isn’t Just About Pain-It’s About Function
It’s easy to think of hip osteoarthritis as just a pain problem. But the real issue is what that pain steals from you: walking to the mailbox, playing with your grandkids, climbing stairs, even getting out of a chair. A 2024 Nature study tracked 65-year-old adults with hip OA and obesity. Those who lost more than 10% of their body weight didn’t just feel less pain-they regained their lives.
The biggest improvement? Quality of life. Not just pain scores. Not just mobility. Their ability to do daily activities without fear or limitation jumped by 31%. That’s not a small tweak. That’s life-changing. And it wasn’t just a few people. This was a clear dose-response relationship: the more weight lost, the better the outcome. Losing 5% helped. Losing 7% helped more. Losing 10% or more? That’s when you start seeing real, measurable gains in function, stiffness, and even sports and recreation.
Compare that to knee osteoarthritis, where weight loss has been a gold standard for years. Hip OA was thought to be different-less responsive, less affected by weight. But this study flips that idea. Yes, the hip joint doesn’t bear weight the same way the knee does. But when you carry 20 extra pounds, every step still pushes down on your hip. And over time, that adds up. Losing weight doesn’t just take pressure off-it reduces the whole-body inflammation that’s fueling the joint breakdown.
Why Some Studies Say Weight Loss Doesn’t Help the Hip
So why the confusion? Why does one study say it works, and another says it doesn’t?
In 2023, a randomized trial compared a very-low-calorie diet plus exercise to exercise alone in 101 people with hip OA. At six months, there was no difference in pain levels between the two groups. The group that lost more weight didn’t report less pain. That’s the study that fueled the NEJM Journal Watch headline.
But here’s the catch: they looked at pain at six months. Not at 12.
When they checked again a year later, everything changed. The group that lost weight showed better scores on pain, function, and overall hip improvement. The benefits didn’t show up right away. They took time. That’s the key. Weight loss isn’t a quick fix. It’s a slow, steady reset for your body. The joint needs months to respond. Muscles need time to rebuild. Inflammation doesn’t vanish overnight.
Also, the study didn’t measure quality of life-the same measure that showed the biggest jump in the Nature study. Pain is just one part of the picture. If you can walk further, climb stairs without stopping, or sleep through the night because your hip isn’t screaming, that’s a win-even if your pain score didn’t drop by a full point.
What’s the Right Amount of Weight to Lose?
You’ve heard “lose 5%” for knee OA. That’s the usual recommendation. But for hip OA, that might not be enough.
The Nature study showed that 10% weight loss was the turning point. That’s not a guess. That’s data. People who lost 10% or more had improvements across every single domain measured: pain, stiffness, daily function, sports, and quality of life. Those who lost less than 5%? Barely moved the needle.
And here’s the kicker: losing 20% didn’t give you much more than losing 10%. A 2023 review in the Journal of Metabolic Health found no significant difference between those who lost 10% versus 20%. That means there’s a sweet spot. You don’t need to become skinny. You just need to lose enough to break the cycle of inflammation and mechanical stress.
For someone weighing 200 pounds, that’s 20 pounds. For someone at 250, it’s 25. It’s not about the number on the scale. It’s about crossing that 10% threshold.
How to Actually Lose Weight When Your Hip Hurts
Okay, so you’re convinced. But how do you lose weight when walking is painful? How do you exercise when every step feels like grinding glass?
The answer isn’t more pain. It’s smarter movement.
First: ditch the idea that you need to run or do high-impact workouts. You don’t. Low-impact options work better-and are safer.
- Swimming or water aerobics: The water supports your weight, reduces joint stress, and builds strength.
- Cycling (stationary or outdoor): Keeps the hip moving without pounding.
- Seated resistance training: Use bands or light weights while sitting. Strengthen your glutes and quads-they’re your hip’s natural shock absorbers.
- Physical therapy: A good PT will design a program that builds strength without aggravating your hip. They’ll also teach you how to move in ways that protect your joint.
And diet? It’s not about starving yourself. It’s about eating differently.
A 2023 review found that low-carbohydrate diets, when combined with exercise, led to better outcomes than exercise alone. That doesn’t mean going keto overnight. It means cutting out sugary drinks, white bread, pastries, and processed snacks. Focus on whole foods: vegetables, lean proteins, healthy fats, beans, nuts, and whole grains. Eat to fuel movement-not to numb discomfort.
The OAHWFL program in Australia and New Zealand-a structured 18-week plan combining diet and exercise-was designed for knee OA. But when adapted for hip OA, it worked. People lost 7-10% of their weight. They moved better. They felt better. And they kept it off.
Joint Preservation: It’s Not Just About Delaying Surgery
People with hip osteoarthritis often hear one thing: “Eventually, you’ll need a replacement.” But that’s not the only path.
Weight loss isn’t just about feeling better today. It’s about preserving your joint for tomorrow. Every pound you lose reduces the load on your hip by 4 pounds. That’s physics. That’s biology. That’s time.
Think of it this way: if you lose 20 pounds, you’re taking 80 pounds of pressure off your hip with every step. Over a year, that’s millions of fewer pounds of force grinding on your cartilage. That’s not magic. That’s science.
And it’s not just mechanical. Fat tissue isn’t just padding. It’s active tissue that produces inflammatory chemicals. The more fat you carry, the more inflammation you’re feeding into your joint. Losing weight lowers those chemicals. It calms the fire inside your hip.
That’s why joint preservation isn’t just a buzzword. It’s a real possibility-for many people, even those with moderate to severe OA. Surgery isn’t the only endgame. Sometimes, it’s the last resort.
What About Medications or Weight Loss Pills?
There are FDA-approved weight loss drugs for people with obesity and OA. But they’re not first-line. They’re for people who’ve tried diet, exercise, and behavior changes for at least six months-and still haven’t reached their goal.
And even then, they’re not a magic bullet. They work best when paired with lifestyle changes. You can’t just pop a pill and eat whatever you want. The drugs help you lose weight faster. But the real benefit comes from what you do after you lose it.
The American College of Rheumatology conditionally recommends weight loss for anyone with hip OA who has overweight or obesity. That’s not a strong recommendation. But it’s a clear one. And it’s based on evidence-not opinion.
Real People, Real Results
In 2012, a study followed 35 people with hip OA and a BMI over 25. They did an 8-month program of exercise and weight loss. They lost an average of 10% of their body weight. Their physical function improved by 32.6%. Pain dropped. Walking speed increased. They could do things they hadn’t done in years.
There was no control group. No placebo. Just real people, making real changes.
One participant, a 68-year-old woman from Brisbane, told her PT: “I didn’t realize I could still dance with my grandkids. I thought that was over.” She lost 18 pounds. She started dancing again. She didn’t need surgery.
That’s not rare. It’s repeatable.
What If You Can’t Lose Weight?
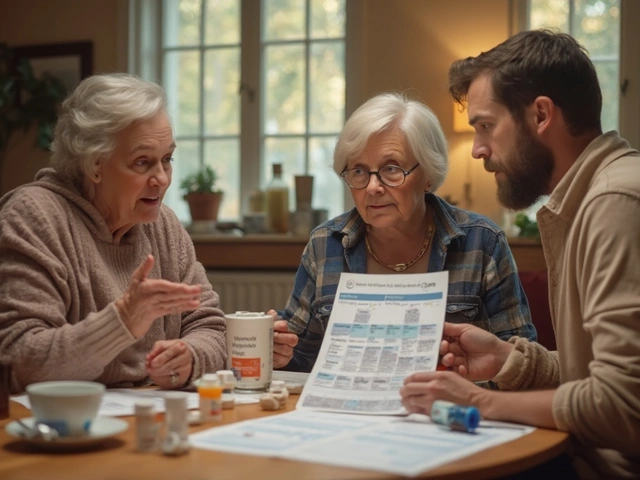
It’s not easy. If you’re in pain, tired, or discouraged, it’s normal to feel stuck.
But you don’t have to do it alone.
Telehealth programs are now available in Australia and New Zealand that connect you with dietitians and physiotherapists who specialize in OA. They’ll adjust your plan based on your pain levels, mobility, and goals. No judgment. No pressure. Just support.
Start small. Walk for 10 minutes a day. Swap soda for water. Add one vegetable to dinner. Build from there. Progress isn’t linear. Some weeks you’ll feel strong. Others, you’ll feel like you’re back at square one. That’s okay.
The goal isn’t perfection. It’s progress. And even a 5% loss can be a step forward. But if you can hit 10%? That’s when the real change begins.
Your hip doesn’t need to be perfect. It just needs to be protected. And weight loss is one of the most powerful tools you have to do that.
Can losing weight really help hip osteoarthritis, or is it just for knee pain?
Yes, losing weight helps hip osteoarthritis-but the effects are different than with knee OA. While knee pain often improves quickly with weight loss, hip improvements take longer and are more about function and quality of life than just pain reduction. A 2024 study found that losing 10% or more of body weight led to significant improvements in hip-related quality of life, daily function, and pain, even if the pain score didn’t drop dramatically at first.
How much weight do I need to lose to see results with hip OA?
Losing 5% of your body weight helps, but the biggest benefits kick in at 10% or more. Studies show that people who lost 10% or more had clinically meaningful improvements in pain, stiffness, walking ability, and overall quality of life. Losing 20% didn’t give much more benefit than 10%, so aiming for 10% is a realistic and powerful target.
What’s the best way to lose weight when my hip hurts too much to walk?
You don’t need to walk to lose weight. Try swimming, cycling, seated strength training, or water aerobics-all low-impact options that protect your hip while building strength. Pair that with a diet focused on whole foods, less sugar, and fewer processed carbs. Programs like OAHWFL, adapted for hip OA, combine structured diet plans with tailored exercise and have helped people lose 7-10% of their weight safely.
Will losing weight delay or prevent the need for hip replacement surgery?
Yes, for many people. While surgery may still be needed eventually, losing weight reduces the mechanical stress on your hip joint and lowers inflammation, which can slow the progression of osteoarthritis. This can delay surgery by years-or in some cases, avoid it altogether. The goal isn’t to fix the joint completely, but to preserve it as long as possible.
Are weight loss medications a good option for hip OA?
Weight loss medications are an option for people with obesity (BMI ≥30) who haven’t succeeded with lifestyle changes after six months. They’re not a shortcut-they work best when combined with diet and exercise. They’re not first-line treatment. Lifestyle changes are still the most effective, safest, and longest-lasting approach for managing hip osteoarthritis.
If you’re living with hip osteoarthritis and carrying extra weight, you’re not powerless. You’re not doomed to surgery. You’re not stuck. The science is clear: losing weight-especially 10% or more-can change the trajectory of your condition. It’s not about being thin. It’s about being strong. About moving freely. About living without fear. And it starts with one step. Even if it’s a small one.




14 Comments
JAY OKE-25 November 2025
Been living with hip OA for 6 years. Lost 18 lbs last year by swapping soda for sparkling water and doing pool workouts. Didn’t feel magic overnight, but now I can walk to the store without wincing. 10% really is the threshold.
Still can’t dance like I used to, but I’m not crying about it anymore.
Joe bailey-27 November 2025
Yo, this is the kind of post that actually gives hope. Not ‘just lose weight’ nonsense but real science with real people. I’m 62, 240 lbs, and thought my hip was a goner. Started swimming 3x a week and cutting out white bread. Lost 12 lbs in 4 months. My dog noticed I’m moving better. She doesn’t wag her tail as much when I get up now… which means I’m doing something right.
Keep going. You got this.
Stephen Adeyanju-27 November 2025
THEY DON’T WANT YOU TO KNOW THIS BUT WEIGHT LOSS IS A BIG PHARMA SCAM TO KEEP YOU ON PAINKILLERS AND EVENTUALLY SURGERY
THEY MAKE BILLIONS OFF HIP REPLACEMENTS AND THEY’RE SCARED YOU’LL FIGURE OUT YOU CAN FIX THIS YOURSELF WITH WATER AND CHICKEN BREASTS
THEY’RE LYING TO YOU ABOUT ‘IT DOESN’T WORK’ BECAUSE THEY CAN’T PROFIT FROM IT
james thomas-28 November 2025
Look, if you’re obese and have hip OA, you’re not a victim-you’re a liability to your own biology. The fact that people still need studies to prove that fat is inflammatory is honestly embarrassing. This isn’t rocket science. It’s physiology. If your body is literally burning itself from the inside out because of adipose tissue, then yes, losing weight isn’t ‘helpful’-it’s survival.
Also, ‘low-carb’ isn’t keto. Stop acting like it’s a cult. Eat food. Not garbage. Done.
Cynthia Springer-29 November 2025
I’m curious-how many of the studies controlled for muscle mass? I’ve seen people lose weight but also lose lean tissue, which can actually worsen joint stability. And what about sarcopenic obesity? Is the 10% threshold adjusted for age or baseline strength?
Also, did any of the trials track long-term weight maintenance? I’m worried about the rebound effect.
Brittany Medley-30 November 2025
As a physical therapist who’s worked with 200+ hip OA patients, I can say this: the ones who lost 10%+ didn’t just ‘feel better’-they stopped asking for pain meds. They started walking their dogs again. They slept through the night. The pain scores didn’t always change much, but their lives did.
And yes, it takes time. Six months minimum. But if you’re patient, your hip will thank you. Not with a hug, but with less screaming.
Ali Miller- 1 December 2025
AMERICA IS WEAK. WE LET CORPORATE MEDICINE TELL US TO TAKE PILLS INSTEAD OF DOING THE WORK.
IN RUSSIA, THEY JUST TELL YOU TO WALK OR DIE. NO EXCUSES. NO THERAPISTS. NO ‘LOW IMPACT.’ JUST WALK.
WE’RE A NATION OF CRYBABIES WHO THINK WATER AEROBICS IS ‘EXERCISE.’
YOU WANT TO FIX YOUR HIP? STOP BEING A COWARD.
mohit passi- 2 December 2025
Life is a series of small rebellions against gravity.
Every step you take while overweight is a silent betrayal of your own body.
But when you lose 10%? That’s not weight loss.
That’s reclaiming your right to move.
Not to be ‘fit.’ Not to look good.
But to feel alive.
And that? That’s worth every sweat drop.
🫡
Aaron Whong- 2 December 2025
It’s fascinating how the biomechanical load reduction model is being conflated with systemic inflammatory modulation-two distinct pathophysiological pathways that, while synergistic, are not isomorphic.
Furthermore, the reliance on self-reported QoL metrics introduces significant recall bias, particularly in populations with comorbid depression or sedentary lifestyle-induced anhedonia.
Until we control for adipokine profiles and synovial fluid cytokine concentrations, any claim of ‘clinically meaningful improvement’ remains epistemologically suspect.
Sanjay Menon- 3 December 2025
How quaint. A 2024 Nature study? How pedestrian. The real breakthroughs are in gene therapy and CRISPR-edited chondrocytes. This ‘lose 10%’ advice is like recommending a Band-Aid for a broken femur.
And don’t get me started on ‘water aerobics.’ That’s not fitness-that’s aquatic performance art for people who’ve given up.
Real people don’t swim to fix their hips. Real people fix their hips with precision medicine.
Marissa Coratti- 4 December 2025
While I deeply appreciate the empirical rigor of the referenced studies, I must emphasize that the longitudinal nature of these interventions cannot be overstated. The physiological adaptations-including reduced circulating interleukin-6, improved insulin sensitivity, and enhanced neuromuscular coordination-are not instantaneous phenomena, but rather emergent properties of sustained behavioral change over a minimum of six to twelve months.
Furthermore, the psychological dimension-particularly the restoration of self-efficacy and reduction of fear-avoidance behaviors-plays a pivotal role in functional recovery, which is often underrepresented in quantitative metrics.
Therefore, I urge all individuals to approach this journey not as a short-term weight-loss endeavor, but as a lifelong commitment to holistic musculoskeletal integrity.
Amanda Wong- 5 December 2025
So let me get this straight. You’re telling me that after decades of doctors telling us to lose weight, we finally have ‘science’ that says… we should lose weight?
And this is a revelation? Where was this study when I was told to ‘just walk it off’ in 2008?
Also, why is everyone acting like this is new? My grandma lost weight in the 70s and walked better. No study needed.
Also, I’m not losing 10% of my body weight. I’m not a lab rat.
Kaushik Das- 5 December 2025
Bro, I lost 22 lbs after my hip started clicking like a rusty hinge. Didn’t do anything fancy. Just stopped eating midnight biryani and started doing chair squats while watching Netflix.
Now I can play kabaddi with my nephews without crying. My wife says I’m ‘less grumpy.’
10% ain’t magic. It’s just… not being a dumbass anymore.
Also, water aerobics? Sounds like a yoga class for turtles. But hey, if it works, I’m not judging.
Brittany Medley- 5 December 2025
Replying to @4889: You said you can walk to the store now-that’s huge. But don’t underestimate the little wins. I had a patient who started by just standing up from her chair without using her arms. Took her 3 weeks. But that was the first step to walking to the mailbox.
Progress isn’t always visible. But it’s always happening.
Keep going. You’re not just losing weight. You’re rebuilding your independence.