When you start ADHD medication, the goal is simple: focus better, feel calmer, get through the day. But for many families, a quiet worry lingers - are these drugs safe long-term? Especially when it comes to the heart and sleep. The truth isn’t black and white. Stimulants like Ritalin, Adderall, and Vyvanse work - for about 70 to 80% of people with ADHD. But they’re not harmless. And understanding the real risks - not the fear-driven headlines - is what matters most.
How Stimulants Affect the Heart
Stimulants for ADHD boost dopamine and norepinephrine in the brain. That’s how they improve attention. But those same chemicals also hit the heart. They make it beat faster and push blood through arteries with more force. That’s why blood pressure and heart rate go up - slightly, but consistently.
A 2025 study from the University of Southampton, the largest of its kind, tracked over 10,000 patients on ADHD meds. The average increase? Just 1 to 4 mmHg in systolic blood pressure. Heart rate climbed by 1 to 2 beats per minute. That’s not a storm. It’s a gentle tide. For most people, it stays that way - stable, manageable.
But here’s where it gets tricky. Over years, that small, steady rise adds up. A 2024 JAMA Psychiatry study followed 14 years of data and found a 17% higher risk of developing high blood pressure or arterial disease in people who took stimulants long-term. The risk rose with higher doses and longer use - especially in the first three years. And a separate 2024 study from the American College of Cardiology found that young adults on stimulants were 57% more likely to develop cardiomyopathy after eight years than those who didn’t take them.
Does that mean everyone should stop? No. The absolute risk is still very low. For every 1,000 people taking stimulants, maybe one or two will have a serious heart issue directly tied to the medication. The number needed to harm is over 1,000. Meanwhile, untreated ADHD carries its own risks - poor school performance, job loss, accidents, substance abuse. The balance tips toward benefit for most.
Not all meds act the same. Methylphenidate and amphetamine-based drugs (like Vyvanse) show similar cardiovascular effects. Even non-stimulants like atomoxetine (Strattera) can raise blood pressure and heart rate - a surprise to many doctors who assume only stimulants do. The one exception? Guanfacine. It actually lowers both.
Who’s at Higher Risk?
Most people handle these meds fine. But some need extra caution.
- Family history of sudden cardiac death - especially before age 40.
- Known heart conditions - like congenital heart defects, arrhythmias, or prior heart failure.
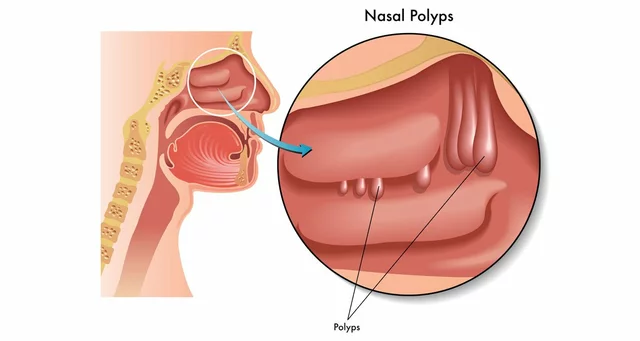
- Long QT Syndrome - a rare electrical problem in the heart. Some ADHD meds are flagged as ‘conditional risk’ by CredibleMeds.org. Not a hard stop, but you need a cardiologist’s input.
- High blood pressure already - stimulants can make it harder to control.
- Teenagers and young adults - their hearts are still developing. The ACC study showed the strongest cardiomyopathy risk in this group.
That’s why guidelines don’t push for universal ECGs anymore. The American Heart Association once recommended them. Now, they say: assess risk first. Ask about chest pain, fainting, palpitations. Check family history. If anything raises a red flag, get an ECG. If not, start low and go slow.
Sleep Problems: The Hidden Cost
If your child can’t fall asleep, or you’re tossing and turning at night, stimulants might be why. About 30 to 50% of people report trouble sleeping when they first start. It’s not just ‘being wired.’ The brain’s arousal system is literally turned up.
Extended-release pills are designed to last all day. But for some, that means the medication is still active 10 or 12 hours later - right when bedtime rolls around. That’s when sleep latency (the time it takes to fall asleep) increases by 15 to 30 minutes on average, according to the American Academy of Sleep Medicine.
Here’s what works:
- Take it earlier. If you’re taking it at 8 a.m., try 7 a.m. instead. Even an hour makes a difference.
- Switch to short-acting. If you’re on Concerta and struggling with sleep, ask about switching to plain methylphenidate taken in the morning and early afternoon.
- Try melatonin. A low dose - 0.5 to 5 mg - taken 1 to 2 hours before bed helps reset the sleep clock. It’s not addictive. It doesn’t interfere with ADHD meds.
- Consider non-stimulants. Atomoxetine doesn’t usually cause insomnia. Guanfacine? It often improves sleep quality - even though it’s not a stimulant.
Many patients find sleep issues fade after a few weeks as their body adjusts. But if it doesn’t? Don’t ignore it. Chronic poor sleep worsens ADHD symptoms. It’s a loop: the med helps focus but hurts sleep, and poor sleep makes focus worse.
Monitoring: What You Should Actually Do
Don’t wait for a crisis. Get ahead of it.
- Baseline check - Before starting any ADHD med, get your blood pressure and heart rate recorded. Keep a note.
- Check every 3 to 6 months - Even if you feel fine. The changes are slow, but they’re real. The American Academy of Pediatrics says this is standard care.
- Track symptoms - Note any chest pain, dizziness, racing heart, or fainting spells. Write them down. Bring them to your doctor.
- Ask about ECG - Not for everyone. But if you have a family history of heart trouble, or you’re over 18 and on high doses, it’s worth discussing.
And here’s something many miss: non-stimulants aren’t risk-free. Atomoxetine can raise blood pressure too. So don’t assume switching to Strattera automatically solves your heart concerns. Monitor all meds the same way.

What’s Changing in 2025?
The field is evolving. The FDA now requires all new ADHD drugs to include long-term cardiovascular safety data. Researchers are building risk calculators that use age, dose, duration, and even genetic markers to predict who’s more likely to have heart issues. One study is testing whether certain DNA patterns make someone more sensitive to stimulant-induced heart rate spikes.
Meanwhile, doctors are getting better at personalizing treatment. If your child has high blood pressure, they might start with guanfacine. If sleep is the biggest problem, they might try a short-acting stimulant with melatonin. If anxiety is high, they might avoid amphetamines altogether.
The message from the American Psychiatric Association’s 2025 guidelines is clear: stimulants remain first-line treatment. But monitoring isn’t optional anymore. It’s part of the prescription.
The Bottom Line
ADHD stimulants are not dangerous for most people. But they’re not harmless either. The cardiovascular risks are small, real, and dose-dependent. Sleep issues are common but often fixable. The key isn’t avoiding these meds - it’s using them wisely.
If you’re considering stimulants: talk to your doctor about your heart history. Get baseline numbers. Track sleep. Don’t just accept insomnia as ‘normal.’ If you’re already on them: keep your appointments. Don’t skip blood pressure checks. If your child is on meds, ask how they’re sleeping. If they’re having trouble, don’t wait until the next visit - call sooner.
These medications change lives. But they’re tools, not magic. Use them with awareness, not fear. And always, always - monitor.
Do ADHD stimulants cause heart attacks?
Heart attacks directly caused by ADHD stimulants are extremely rare. While these medications can slightly raise blood pressure and heart rate, the risk of a heart attack in healthy individuals is very low. Studies show the absolute risk is under 1 in 1,000 patients per year. The bigger concern is long-term strain on the cardiovascular system, especially with high doses or pre-existing conditions. Always get baseline checks and monitor regularly.
Can I take ADHD meds if I have high blood pressure?
Yes - but with caution. Stimulants can make high blood pressure harder to control. Your doctor may start you on a lower dose, choose a non-stimulant like guanfacine or atomoxetine, or add a blood pressure medication. Regular monitoring is essential. Never stop your blood pressure meds to take ADHD drugs. Work with both your psychiatrist and primary care provider to balance both conditions safely.
Why do ADHD meds mess with sleep?
ADHD stimulants increase alertness by boosting dopamine and norepinephrine - the same chemicals your brain uses to stay awake. That’s why they help focus during the day. But if the medication is still active at night, it delays sleep onset. Extended-release versions can cause this 10-12 hours later. Taking the last dose earlier, switching to short-acting forms, or using melatonin can help. Sleep problems often improve after a few weeks, but if they don’t, talk to your doctor.
Are non-stimulant ADHD meds safer for the heart?
Not necessarily. While non-stimulants like atomoxetine and viloxazine don’t act the same way as stimulants, they still raise blood pressure and heart rate in many people - sometimes as much as stimulants. Guanfacine is the exception: it lowers both. So switching from Adderall to Strattera doesn’t automatically mean lower heart risk. Always monitor blood pressure and heart rate regardless of the type of medication you take.
Should my child get an ECG before starting ADHD meds?
Routine ECGs aren’t recommended for all children. Major guidelines from the American Academy of Pediatrics say the risk is too low to justify screening everyone. But if your child has a family history of sudden cardiac death, fainting spells, heart murmurs, or known heart conditions, an ECG is wise. Talk to your pediatrician or a cardiologist. They’ll help decide if it’s needed based on personal risk - not just the diagnosis.
Can I stop ADHD meds if I’m worried about side effects?
Never stop abruptly. Stopping suddenly can cause rebound symptoms - worse focus, irritability, fatigue, or even depression. If side effects concern you, talk to your doctor. They can adjust the dose, change the timing, switch medications, or add support like melatonin for sleep. Most side effects can be managed without quitting. The goal is to find the lowest effective dose that works - not to avoid treatment entirely.




19 Comments
Ashley Elliott- 2 December 2025
I've been on Vyvanse for six years. My BP is a little higher, but my doctor keeps an eye on it. Sleep was rough at first, but melatonin fixed it. I'm not scared-I'm informed.
Chad Handy- 3 December 2025
The data in this post is misleading because it ignores the pharmaceutical industry's influence on clinical guidelines. The 17% increased risk of hypertension sounds small until you realize that the baseline population in these studies is already skewed toward healthier individuals who are more likely to be prescribed stimulants in the first place. Meanwhile, the long-term neurochemical adaptations from chronic dopamine elevation are barely studied beyond five years, yet we're prescribing these drugs to children for decades. The real question isn't whether the heart is affected-it's whether the brain ever fully recovers when the meds stop.
Augusta Barlow- 3 December 2025
They say it's 'safe' but they never tell you who's paying for the studies. Big Pharma funds 90% of ADHD research. The '1 in 1000' risk? That’s the number they want you to believe. Meanwhile, I’ve got three friends whose kids developed arrhythmias after two years on Adderall. No one connects the dots until it’s too late. And now they’re pushing these meds in schools like they’re vitamins. Wake up.
Jenny Rogers- 5 December 2025
It is imperative to underscore that the pharmacological modulation of catecholaminergic systems, while efficacious in the management of attentional dysregulation, carries with it a quantifiable, albeit low-probability, cardiovascular risk profile. One must not conflate statistical insignificance with biological irrelevance. The longitudinal accumulation of hemodynamic stressors, even at subclinical levels, necessitates vigilant monitoring, particularly in developing adolescents. The notion that 'it's fine if you feel fine' is a dangerous fallacy.
zac grant- 6 December 2025
The key here is dose titration and regular vitals. Most docs skip the BP check after the first visit. Big mistake. I’ve seen patients crash their sleep with extended-release meds because they didn’t adjust timing. Melatonin’s underrated-0.5mg works wonders. And yeah, Strattera isn’t magic. BP can still creep up. Monitor everything. Don’t assume.
michael booth- 6 December 2025
Thank you for this clear and balanced overview. It is vital that we approach ADHD treatment with both scientific rigor and human compassion. Monitoring blood pressure and sleep patterns should be standard, not optional. These medications can be life-changing, but only when used with intention and awareness.
Libby Rees- 7 December 2025
I’ve been on methylphenidate since I was 12. I’m 32 now. My BP is fine. I sleep fine. I take it at 7 a.m. and never have issues. I know people who had problems, but they took it late or didn’t tell their doctor about their family history. This isn’t about fear. It’s about responsibility.
Dematteo Lasonya- 8 December 2025
My son started on Adderall last year. Sleep was terrible at first. We tried everything-later doses, no screens, white noise. Nothing worked. Then we switched to short-acting and gave him 1mg melatonin. He’s been sleeping 8 hours straight for months. It’s not perfect, but it’s manageable. I wish we’d known sooner.
Rudy Van den Boogaert- 8 December 2025
I’ve been on Guanfacine for two years. No heart issues. Sleep’s actually better. I used to be on Vyvanse but the jitteriness and insomnia killed me. Guanfacine doesn’t feel like a chemical boost-it feels like calm focus. Worth considering if you’re struggling with side effects.
Gillian Watson- 9 December 2025
In the UK, we’re much more cautious about prescribing stimulants to kids under 16. We start with behavioral therapy first. If meds are needed, we go low and slow. The NHS doesn’t push them like it’s a quick fix. I wish more countries took this approach.
Pavan Kankala-11 December 2025
They’re hiding the truth. The real risk isn’t 1 in 1000-it’s 1 in 100 if you look at the unreported cases. Hospitals don’t list stimulants as the cause because then they’d have to admit they pushed a drug that caused cardiac damage. The system protects itself, not you. Wake up. They’re turning kids into walking heart timers.
Martyn Stuart-11 December 2025
I’ve been a nurse for 20 years, and I’ve seen too many kids on stimulants with no follow-up. Parents think, 'It’s working, so it’s fine.' But what about the silent rise in BP? Or the insomnia that turns into chronic fatigue? You need to track it. Write it down. Bring it to the doc. Don’t wait for a crisis. Prevention > reaction.
Shofner Lehto-12 December 2025
My daughter started on Ritalin at 8. We did the baseline ECG because her uncle had sudden cardiac arrest at 38. Turned out she had a mild long QT. They switched her to guanfacine. She’s doing amazing now. Don’t assume you’re fine. Ask for the test. It takes 15 minutes.
Yasmine Hajar-12 December 2025
I used to be the mom who thought ADHD meds were overprescribed. Then my kid got diagnosed. The difference was night and day-he went from failing classes to getting A’s. But the sleep? Oh god. We cried over bedtime for months. Melatonin didn’t help at first. Then we tried 2mg, 90 minutes before bed, and no screens after 7. It worked. It’s not magic. It’s management.
Rachel Bonaparte-13 December 2025
You know what’s really scary? That this article sounds so reasonable. That’s the trap. They make it sound like a minor trade-off-'a little higher BP, a little insomnia, no big deal.' But what they don’t tell you is that the brain adapts. The dopamine receptors downregulate. The heart gets used to being pushed. And then? You’re dependent. Not just for focus-for normalcy. And if you stop? You’re not yourself. They’re not treating ADHD. They’re creating a lifelong chemical crutch.
Scott van Haastrecht-15 December 2025
I’ve been on Adderall for 11 years. My heart rate is 105 bpm at rest. My BP is 145/92. I’ve had three panic attacks since starting. My doctor says 'it’s fine.' But I’m not fine. I’m terrified to stop because I’ll lose everything I’ve built. And now I’m supposed to be grateful? This isn’t treatment. It’s chemical imprisonment.
Chase Brittingham-15 December 2025
This is the kind of post I wish I’d read before I started. I thought sleep issues were just 'part of it.' Turns out, they’re fixable. I switched to morning-only methylphenidate and started taking melatonin. My sleep improved in a week. My focus didn’t drop. I wish I’d known sooner. Don’t suffer in silence.
Bill Wolfe-17 December 2025
Let’s be real-most people on stimulants aren’t getting monitored. Doctors don’t have time. Parents don’t know to ask. And the pharmaceutical reps? They’re not handing out BP cuffs. The system is built to keep you medicated, not healthy. Guanfacine? It’s the only one that doesn’t make you feel like a robot. But no one talks about it because it’s not profitable. You’re being sold a dream. And the bill comes due in your arteries.
Jordan Wall-18 December 2025
So I’m reading this and I’m like… are we sure these studies are peer-reviewed? The '17% higher risk' sounds legit but the citation is vague. Also, why is there no mention of gut-brain axis? ADHD meds alter microbiome too. And nobody talks about that. Maybe the real issue is inflammation? Just sayin’. Also, did you know guanfacine was originally a hypertension drug? 😏