Bronchodilator Alternatives: What You Need to Know
When considering bronchodilator alternatives, medications or therapies used instead of traditional bronchodilators to open airways. Also known as non‑beta‑agonist options, they give patients more flexibility, especially when standard inhalers cause side effects or lose effectiveness.
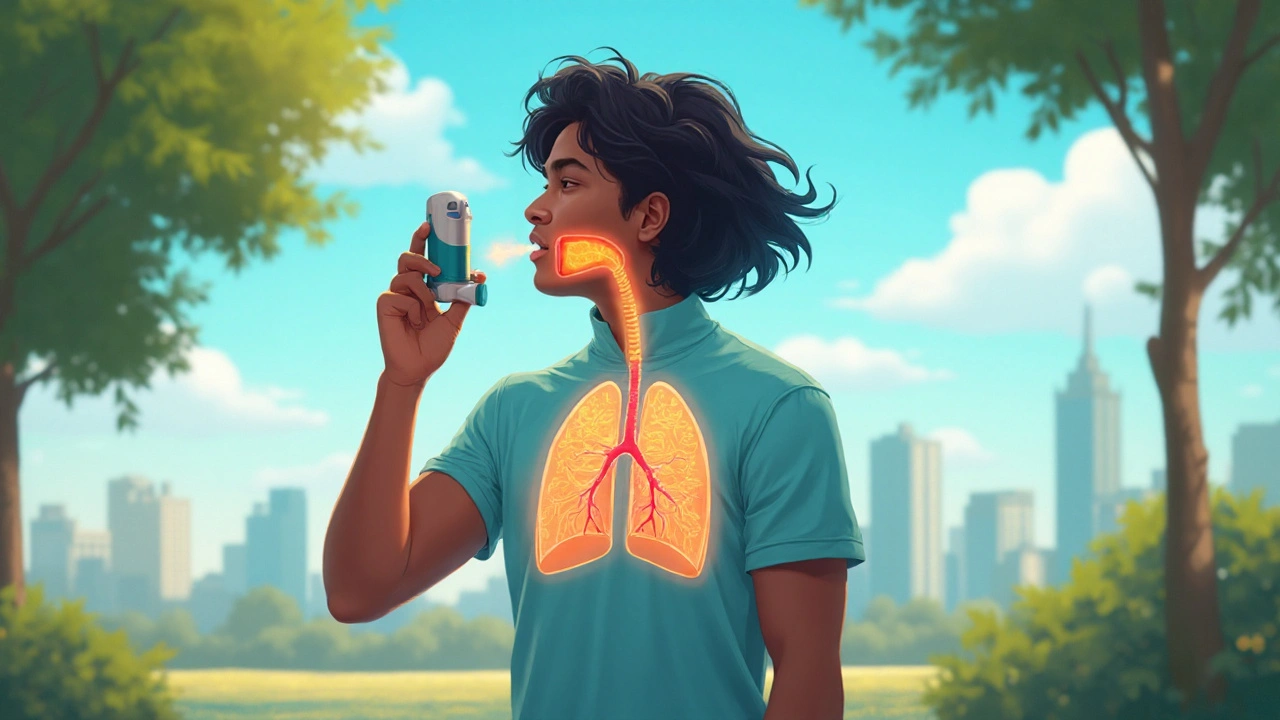
One major class to understand is the Bronchodilator, a drug that relaxes airway smooth muscle to improve airflow. Traditional bronchodilators include short‑acting beta‑agonists (SABAs) like albuterol and long‑acting forms (LABAs) such as salmeterol. While these work fast, they can trigger tremor, tachycardia, or tolerance over time, prompting clinicians to look for alternatives that act via different pathways.
For people with Asthma, a chronic inflammatory disease of the airways characterized by wheezing, shortness of breath, and reversible airflow obstruction, the goal is to control inflammation and prevent attacks. Bronchodilator alternatives like inhaled corticosteroids (ICS), leukotriene receptor antagonists (LTRAs), and biologics (e.g., omalizumab) target the inflammatory cascade rather than just the muscle layer. This shift reduces reliance on rescue inhalers and can lower emergency visits.
Patients with COPD, chronic obstructive pulmonary disease, a progressive condition marked by airflow limitation that is not fully reversible often need a broader toolbox. Long‑acting muscarinic antagonists (LAMAs) such as tiotropium act on the parasympathetic nervous system, offering an alternative to beta‑agonists. Adding phosphodiesterase‑4 inhibitors like roflumilast can further reduce exacerbations, especially in severe cases where standard bronchodilators fall short.
Choosing the right alternative hinges on several attributes: mechanism of action, onset speed, duration, side‑effect profile, and cost. For instance, LAMAs provide a smooth, once‑daily dosing schedule, which many patients prefer over multiple daily SABA doses. Conversely, leukotriene modifiers are taken orally, making them convenient for those who dislike inhalers, but they may be less potent during acute attacks.
How to Match Alternatives to Your Lifestyle and Health Profile
First, assess the primary symptom driver. If rapid relief during an attack is the main concern, a short‑acting non‑beta‑agonist like ipratropium (an anticholinergic) can serve as a rescue agent without the jittery side effects of SABAs. Second, consider comorbidities. Patients with cardiovascular disease often avoid high‑dose beta‑agonists, making LAMA‑based regimens safer. Third, evaluate adherence potential; inhaled powders require proper technique, while oral tablets improve compliance for some users.
Cost is another practical factor. Generic LAMAs and oral LTRAs are frequently covered by insurance plans, while biologics can be expensive but may qualify for patient assistance programs. Understanding these financial dimensions helps avoid interruptions in therapy that could worsen breathing problems.
Device selection ties directly into effectiveness. Metered‑dose inhalers (MDIs) need hand‑breath coordination, which can be tricky for elderly COPD patients. Dry‑powder inhalers (DPIs) rely on sufficient inspiratory flow, which might be insufficient during severe asthma exacerbations. Choosing the right device for the chosen alternative improves drug delivery and reduces waste.
Safety monitoring differs across alternatives. Inhaled steroids demand regular checks for oral thrush, requiring patients to rinse their mouths after use. LAMAs can cause dry mouth, so hydration advice is essential. Biologics may suppress the immune system, so labs are required before each dose.
Clinical guidelines from the Global Initiative for Asthma (GINA) and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) now place bronchodilator alternatives front and center. GINA recommends low‑dose ICS‑formoterol as a preferred reliever in many cases, while GOLD suggests adding a LAMA to any regimen that includes a LABA to reduce exacerbations.
Real‑world experience shows that patients who combine a LAMA with an inhaled steroid often report better symptom control than those relying solely on SABAs. This combination illustrates a semantic triple: Bronchodilator alternatives encompass non‑beta‑agonist options; Asthma management requires bronchodilator alternatives; COPD treatment influences choice of bronchodilator alternatives. Understanding these connections helps clinicians craft personalized plans.
Below you’ll find a curated list of articles that dive deeper into specific drug comparisons, safety tips, and cost‑saving strategies. Whether you’re looking for a side‑by‑side review of inhaler types or want to explore natural adjuncts for breathing health, the collection offers practical insights you can apply right away.
Asthalin (Salbutamol) vs Other Bronchodilators: A Practical Comparison
Explore how Asthalin (Salbutamol) stacks up against other rescue inhalers. Learn mechanisms, pros, cons, and choose the right option for asthma or COPD in clear, practical terms.