Chemotherapy Drug Interactions: What You Need to Know Before Starting Treatment
When you're undergoing chemotherapy, a type of cancer treatment that uses drugs to kill fast-growing cells in the body. Also known as chemo, it's powerful—but it doesn't work in a vacuum. Many other medications, supplements, and even foods can change how it acts in your body, sometimes with serious results. That’s why chemotherapy drug interactions are one of the most overlooked risks in cancer care.
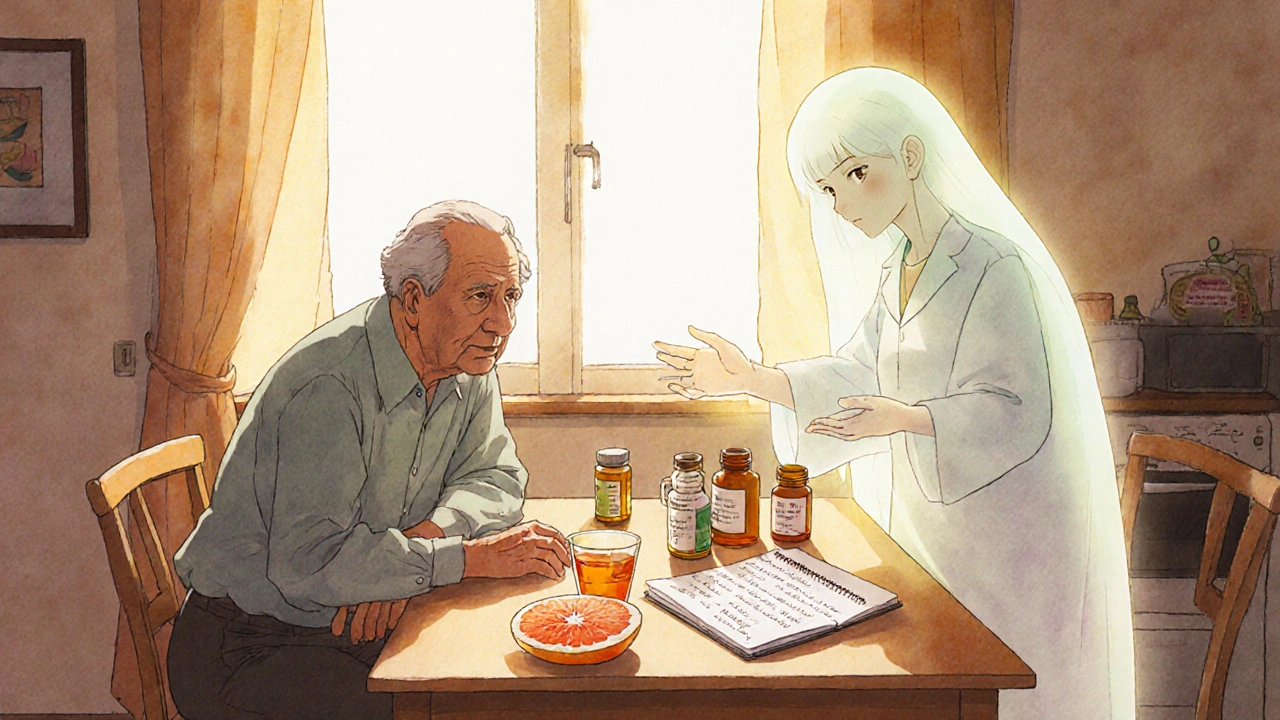
It’s not just about other cancer drugs. Common things like antibiotics, pain relievers, heart meds, and even herbal supplements like St. John’s wort or garlic pills can interfere. For example, some antibiotics can make chemo harder on your liver, while certain antacids can stop your body from absorbing chemo drugs properly. Even something as simple as grapefruit juice can block enzymes your liver needs to process chemotherapy, causing dangerous buildup in your blood. These aren’t rare cases—studies show over 60% of people on chemo take at least one other medication that could interact.
It’s not just about what you take on purpose. Your body’s own changes during treatment matter too. If chemo causes nausea and you start taking an anti-nausea pill, that pill might slow down how quickly your body clears the chemo. Or if you’re dehydrated from fever or vomiting, your kidneys can’t flush out the drugs as well, increasing toxicity. Even something like a common cold can shift how your liver processes chemo. That’s why doctors need a full picture: every pill, every vitamin, every tea you drink. Missing one detail can change your outcome.
Some chemo drugs are especially tricky. Drugs like doxorubicin, paclitaxel, and cisplatin have narrow safety windows—meaning the difference between an effective dose and a toxic one is small. If another drug pushes you over that line, you could end up in the hospital with organ damage, severe infections, or worse. That’s why people on these treatments often get regular blood tests to check liver and kidney function. It’s not just monitoring side effects—it’s catching interactions before they hurt you.
You’re not alone in this. Many others have walked this path, and they’ve learned the hard way. One woman on chemo for breast cancer started taking turmeric supplements for inflammation, not knowing it interfered with her drug’s metabolism. Her white blood cell count dropped dangerously low. Another man took ibuprofen for joint pain and ended up with internal bleeding because it amplified the blood-thinning effect of his chemo. These aren’t hypotheticals—they’re real stories from people who trusted their instincts over professional guidance.
What you’ll find in the posts below are real, practical stories from people who’ve navigated these risks. You’ll see how switching to a generic version of a chemo drug led to unexpected side effects, how a simple herbal remedy clashed with cancer treatment, and why even something like a medical alert bracelet matters when you’re on complex drug regimens. You’ll learn how to talk to your pharmacist about hidden interactions, how to track what you’re taking, and what questions to ask before adding anything new to your routine. This isn’t about fear—it’s about control. Knowing how your drugs interact gives you power over your treatment, not the other way around.
Cancer Medications: Understanding Chemotherapy Drug Interactions and How to Stay Safe
Chemotherapy drug interactions can be life-threatening. Learn which medications, supplements, and foods interfere with cancer treatment-and how to stay safe during therapy.