Drug Interactions with Chemo: What You Need to Know
When you're undergoing chemotherapy, a powerful treatment that targets fast-growing cancer cells. Also known as chemo, it works by disrupting cell division—but it doesn't know the difference between cancer cells and healthy ones. This is why even small changes in your other medications can lead to serious, sometimes life-threatening, drug interactions with chemo, when other substances change how chemotherapy is absorbed, processed, or eliminated by your body.
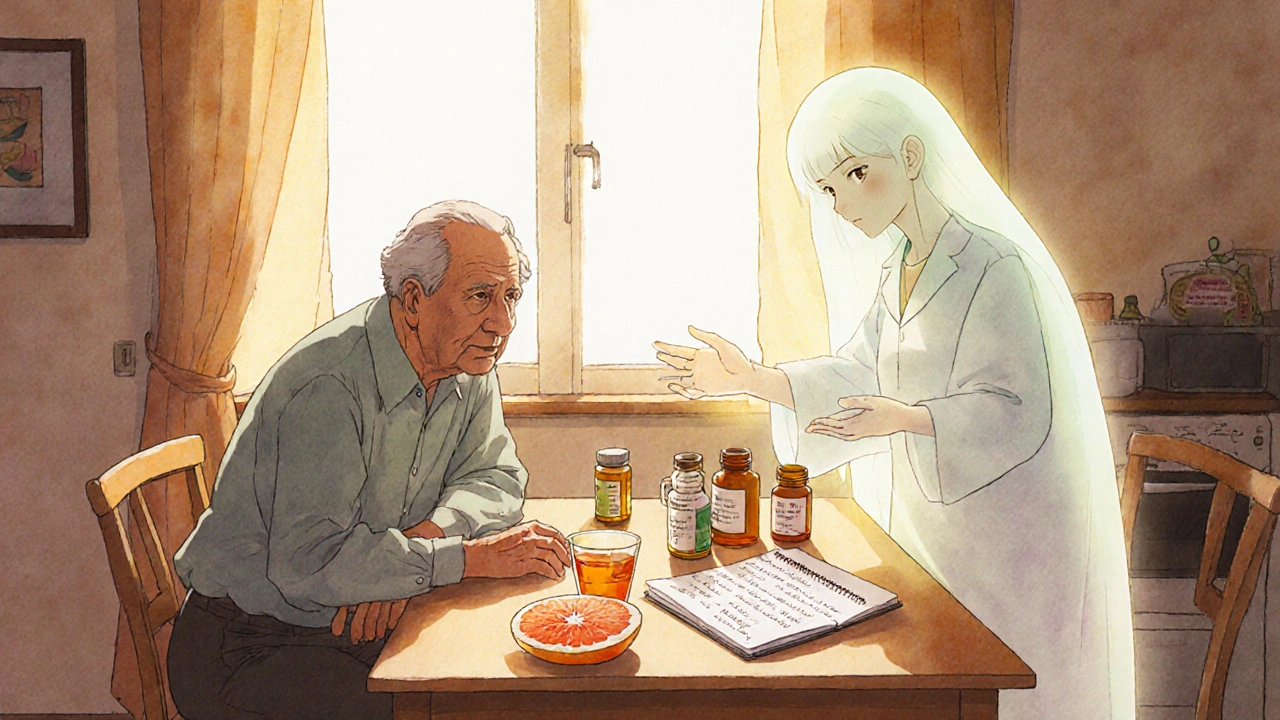
These interactions aren't rare. A 2021 study in the Journal of Clinical Oncology found that over 60% of cancer patients were taking at least one medication that could interfere with their chemo. Common culprits include over-the-counter painkillers like ibuprofen, herbal supplements like St. John’s wort, and even antacids. Some drugs make chemo less effective; others make it more toxic. For example, taking aspirin or naproxen while on certain chemo drugs can increase bleeding risk. Grapefruit juice can block enzymes that break down chemo, causing dangerous buildup in your blood. Even something as simple as an antibiotic like erythromycin can alter how your liver handles chemotherapy, raising your chances of severe side effects.
It’s not just about prescription drugs. supplements, including vitamins, minerals, and herbal products marketed as "natural" or "immune-boosting". Also known as nutraceuticals, they often lack regulation and can interfere with chemo in unpredictable ways. Vitamin C in high doses might reduce the effectiveness of some chemo drugs. Milk thistle, often used for liver support, can alter how your body metabolizes chemotherapy. And melatonin, taken for sleep, can interact with drugs that affect your immune system. The problem? Many patients don’t tell their oncologist they’re taking these because they assume they’re safe. That’s a mistake.
Even your diet matters. High-sodium foods can worsen fluid retention caused by some chemo drugs. Alcohol can increase liver stress when your body is already working hard to process treatment. And dehydration from not drinking enough water can make kidney damage from chemo more likely. It’s not about being perfect—it’s about being aware. Your care team needs to know everything you’re taking, including doses and timing.
Some patients worry about switching to generics during chemo. While generics are usually safe, inactive ingredients, like fillers, dyes, or preservatives in pills. Also known as excipients, they can trigger reactions in sensitive people. If you’ve had a bad reaction to a brand-name drug, ask if the generic version has the same non-active components. You might need to stick with the original—or find another alternative.
And don’t forget about your medical alert bracelet. If you have a severe allergy to a chemo drug or a reaction to an inactive ingredient, wearing one can save your life in an emergency. It tells paramedics what not to give you when you can’t speak for yourself.
Below, you’ll find real stories and practical advice from people who’ve been through this. We cover what to ask your doctor, which supplements to avoid, how to track your meds, and what signs mean it’s time to call for help. No fluff. Just what you need to stay safe while fighting cancer.
Cancer Medications: Understanding Chemotherapy Drug Interactions and How to Stay Safe
Chemotherapy drug interactions can be life-threatening. Learn which medications, supplements, and foods interfere with cancer treatment-and how to stay safe during therapy.