Salbutamol – Fast‑Acting Bronchodilator Overview
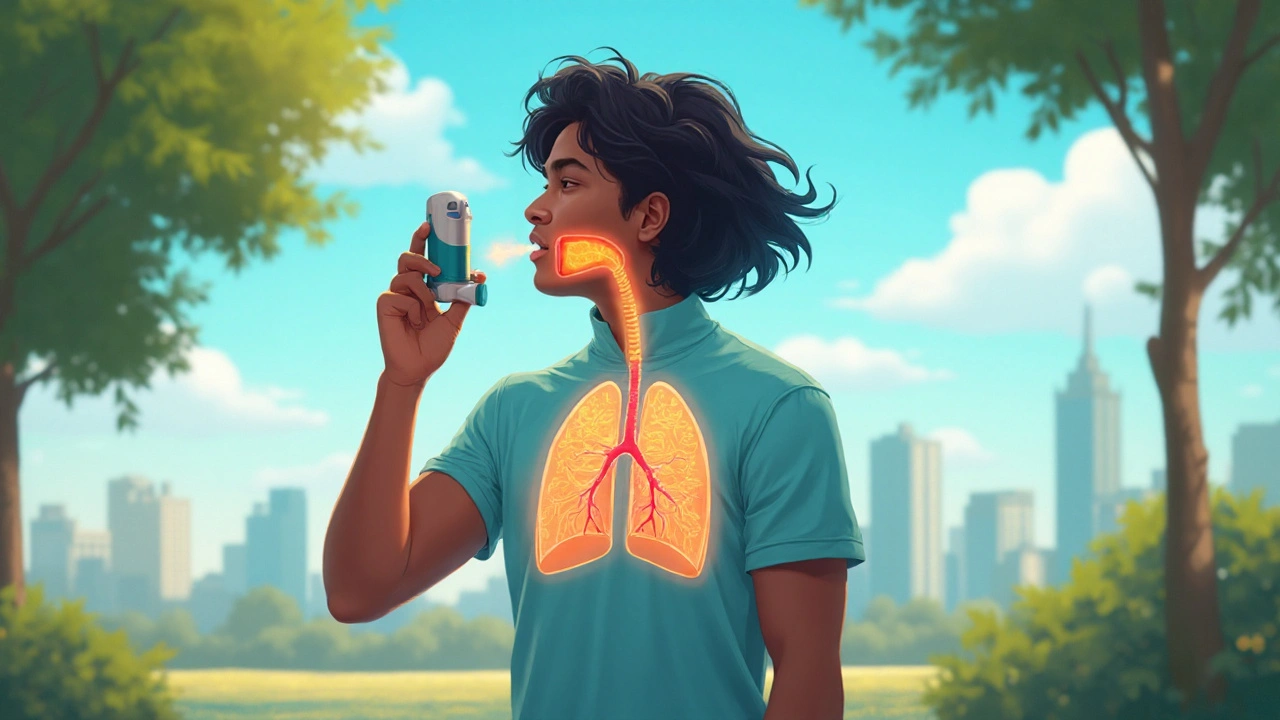
When working with Salbutamol, a fast‑acting bronchodilator that opens airway muscles in minutes. Also known as Ventolin, it belongs to the short‑acting beta2‑agonist class. Salbutamol is the go‑to rescue drug for people who need rapid relief from breathing trouble.
The main condition it treats is Asthma, a chronic inflammatory disease of the airways that causes wheezing and breathlessness. When an asthma flare spikes, the airway muscles tighten, and Salbutamol steps in to relax them. This direct link – Salbutamol relieves asthma symptoms – makes the drug a cornerstone of everyday asthma management.
Delivery matters, and most patients use a handheld Inhaler, a portable device that delivers medication directly into the lungs. The inhaler turns a liquid dose into a fine mist that reaches the bronchi within seconds. Proper technique ensures the full dose lands where it’s needed, turning the device into a life‑saving tool.
From a pharmacology angle, Salbutamol is a Beta2‑agonist, a class of drugs that relax smooth muscle in the bronchi. This class works by binding to beta2 receptors, triggering a cascade that opens the airway. Knowing that Salbutamol is a short‑acting beta2‑agonist helps clinicians choose it for quick relief while reserving long‑acting agents for maintenance.
Like any medicine, Salbutamol can produce Side Effects, unwanted reactions that can occur after taking a medication. The most common are a jittery feeling, rapid heartbeat, and mild tremor. These effects are usually brief, but recognizing them lets users adjust dosage or seek medical advice if they become severe.
Dosage guidelines differ by age and severity. For adults, a typical rescue inhalation is 100‑200 µg, repeatable every 4‑6 hours up to a maximum of 800 µg per day. Children aged 4‑11 years usually start at 100 µg per actuation, with the same frequency limits. Knowing the exact numbers helps avoid under‑ or over‑treatment, especially during an attack.
Salbutamol doesn’t work in isolation. It can interact with other bronchodilators, corticosteroids, and certain heart medications. Combining it with a long‑acting beta2‑agonist may increase heart‑rate effects, while simultaneous use of diuretics can raise the risk of low potassium. Being aware of these interactions lets patients and doctors plan safe regimens.
In emergency situations—like a sudden asthma attack—Salbutamol is the first line of defense. A rapid‑acting inhaler or a nebulizer can reverse airway tightening within minutes, buying precious time before further medical care. This emergency role underscores why many health systems stock it in ambulances and clinics.
Availability varies worldwide. Brand names like Ventolin or Proventil sit beside generic versions that cost less but work the same. In some countries the drug is over‑the‑counter for adults, while others require a prescription. Understanding local access options helps patients stay stocked and avoid interruptions.
Guidelines such as the Global Initiative for Asthma (GINA) recommend Salbutamol as the preferred rescue medication, but they also stress that patients should have an action plan and regular follow‑up. Aligning personal use with these evidence‑based recommendations improves long‑term control and reduces hospital visits.
Practical tips can make a big difference: shake the inhaler before use, exhale fully, place the mouthpiece correctly, inhale slowly while pressing the canister, then hold the breath for about 10 seconds. Cleaning the device weekly prevents clogging and ensures each puff delivers the correct dose.
Below you’ll find a curated collection of articles that dive deeper into Salbutamol’s mechanisms, compare it with other treatments, discuss safety nuances, and offer real‑world advice for getting the most out of this essential medication.
Asthalin (Salbutamol) vs Other Bronchodilators: A Practical Comparison
Explore how Asthalin (Salbutamol) stacks up against other rescue inhalers. Learn mechanisms, pros, cons, and choose the right option for asthma or COPD in clear, practical terms.