Imagine taking a pill because the label says "take daily," but you don’t know if that means once a day or every day. Now imagine you can’t read English at all. This isn’t rare. Across the U.S., millions of people struggle to understand their medication instructions because they’re written in a language they don’t speak. And the consequences? Mistakes. Hospital visits. Even death.
Why Language Barriers Kill
People who don’t speak English well are 1.5 to 3 times more likely to have a dangerous medication error than those who do. That’s not a small risk. It’s life-or-death. A 2006 study by the Institute of Medicine found this pattern clearly. Since then, research has only confirmed it. A 2018 study from the University of California showed that when prescriptions are translated properly, medication errors drop by up to 62%. That’s not a theory-it’s measurable, proven safety.But here’s the problem: most pharmacies still hand out English-only labels. A 2021 survey found only 57% of community pharmacies provide translated prescription instructions. That means more than 4 in 10 patients are left guessing. And guessing with medicine isn’t just risky-it’s deadly.
What Goes on the Label Matters
A prescription label isn’t just a piece of paper. It’s your instruction manual. But most labels use medical jargon like "SIG: Take one tablet by mouth twice daily." Even English speakers struggle with that. For someone who speaks Spanish, Vietnamese, or Arabic, it’s impossible.Effective labels don’t translate words-they translate meaning. The ConcordantRx project created simplified instructions in Chinese, Korean, and Russian that used plain language and clear visuals. The result? 100% of patients understood their instructions. Compare that to the 45% comprehension rate with standard translations. That’s not a small improvement. That’s a revolution.
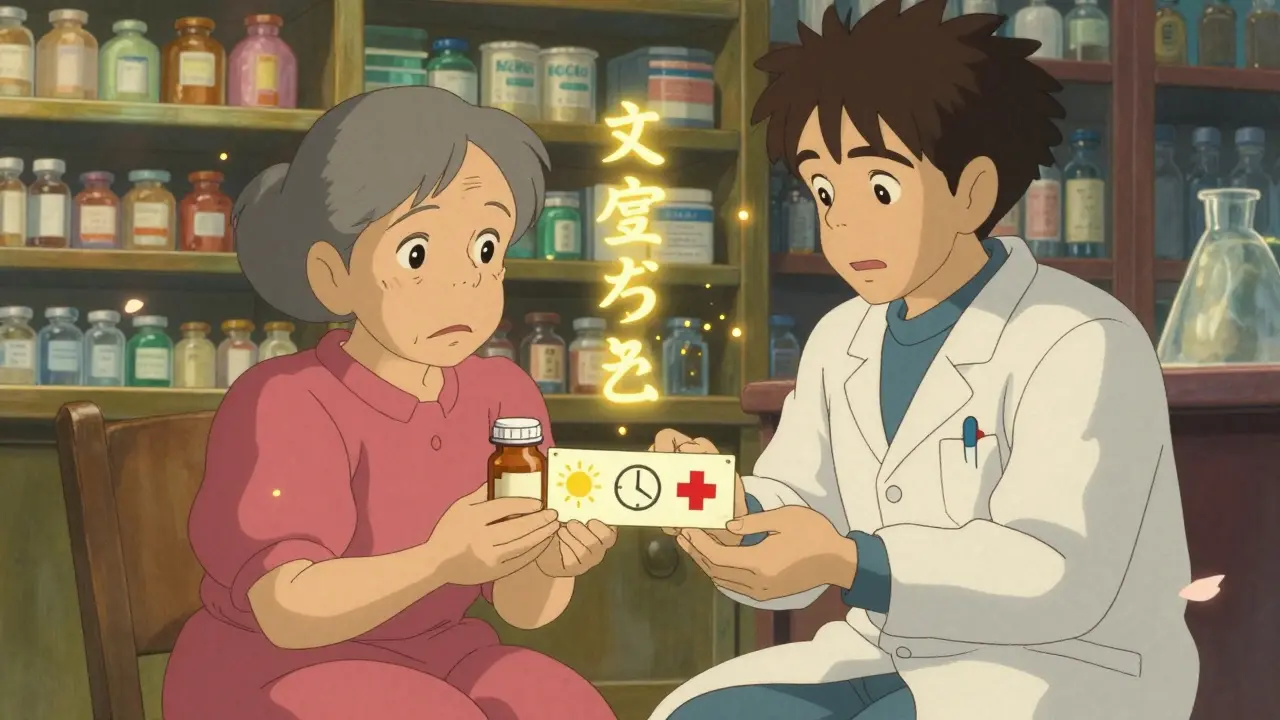
Good labels follow three rules:
- Use plain language-no higher than a 6th-grade reading level.
- Include universal symbols, like a red cross for "avoid alcohol" or a sun for "take in daylight." These follow ISO 3864 and FDA guidelines.
- Never just translate word-for-word. "Take as directed" becomes "Take one pill every morning after breakfast."
Translation That Works vs. Translation That Fails
Not all translations are created equal. There are three main types-and only one saves lives.Family members or friends translating-this is the most common, and the most dangerous. A 2022 report from the Institute for Safe Medication Practices found this method leads to 65% more errors. Why? People don’t know medical terms. They guess. One patient thought "nebulizer solution" was "syringe juice" and drank it.
Automated tools like Google Translate-these are fast and cheap, but dangerously inaccurate. A 2020 FDA review found automated translations had a 38% error rate. AI tools today still make the same mistakes. A 2023 FDA warning said unvalidated AI translations had 43% error rates. That’s worse than flipping a coin.
Professionally translated, medically reviewed labels-this is the only safe option. Companies like RxTran, TransPerfect Healthcare, and LanguageLine Solutions use certified medical translators who understand drug names, dosages, and side effects. Their labels are tested with real patients. Results? 95-100% comprehension. That’s the gold standard.

It’s Not Just Labels-It’s the Whole System
A translated label alone isn’t enough. Medication safety needs a full system.Studies show the best outcomes come from combining three things:
- Bilingual labels-89% of patients understand them.
- Professional interpreters-92% comprehension when a trained interpreter explains the medicine in person.
- Culturally tailored education-85% understanding when materials use familiar examples, like comparing pill schedules to meal times.
One pharmacy in New York started using this three-part system. Within six months, medication errors dropped by 58%. Adherence went up 37%. Patients stopped calling the pharmacy confused. Staff stopped feeling guilty.
Why Aren’t More Pharmacies Doing This?
The answer is simple: cost and complexity.Professional translation costs $2.50 to $5.00 per prescription. For a small pharmacy filling 500 prescriptions a week, that’s $1,250 to $2,500 extra per week. Many say they can’t afford it.
But here’s the truth: not doing it costs more. Medication errors lead to emergency room visits, hospital stays, and lawsuits. A 2023 University of Florida study found pharmacies with strong language access saved 15% on medication-error-related costs. They also saw 22% higher patient satisfaction.
Another barrier? Technology. Only 32% of pharmacies have their translation system connected to their pharmacy software like Rx30 or PioneerRx. That means staff have to manually print translated labels. It’s slow. It’s easy to forget. It’s error-prone.
And training? Most staff get zero cultural competency training. In California, the law requires 8 hours. In most states? Nothing.
What’s Changing-and What’s Coming
Change is happening, but slowly.California now requires pharmacies to provide translations for the top five non-English languages spoken in their area. New York City requires translations for the top 10. Federal law under Title VI of the Civil Rights Act has required this since 2000-but enforcement is weak.
In 2024, new rules are kicking in:
- California’s mandatory language access certification for pharmacies.
- Medicare Part D plans must now report how well they serve non-English speakers.
- Electronic health records will soon auto-detect language preference and trigger translation tools.
By 2026, experts predict 85% of pharmacies will have some kind of language access system. The market for translation services is growing fast-projected to hit $490 million by 2027.
But here’s the catch: languages like Hmong, Navajo, and Somali still have almost no certified medical translators. There are only 12 certified medical interpreters for Navajo nationwide. That’s a gap no app can fix.

What You Can Do Right Now
If you or someone you care for doesn’t speak English well, here’s how to protect yourself:- Ask for translation-Don’t wait. Say, "I need my prescription instructions in my language. Can you help?"
- Ask if they use certified translators-Not Google Translate. Not a family member. Ask: "Is this translation reviewed by a medical professional?"
- Ask for a verbal explanation-Even with a translated label, ask the pharmacist to explain it out loud. If they don’t have an interpreter, ask for one.
- Use visual aids-Ask for pictures or diagrams. A pill with a clock next to it? That’s clearer than "once daily."
- Report problems-If you got wrong instructions and had a bad reaction, tell the pharmacy. File a complaint with your state’s board of pharmacy. Your voice changes things.
Patients Are Speaking Up
On Reddit, a pharmacist wrote: "I had a Korean patient taking their blood thinner twice a day because the label said 'daily' and they thought it meant every day." That’s not a mistake-it’s a system failure.On Healthgrades, patients say: "Staff didn’t check if I understood." "Instructions weren’t in my language." "I was too scared to ask."
One woman from Vietnam told her story: "I took my diabetes pill at night because the label said 'take at bedtime.' I didn’t know 'bedtime' meant before sleeping, not after dinner. My blood sugar crashed. I ended up in the ER."
These aren’t isolated cases. They’re symptoms of a broken system.
Clear Instructions Save Lives
Medication safety isn’t just about pills. It’s about dignity. It’s about respect. It’s about giving people the information they need to stay alive.Translated labels aren’t a luxury. They’re a necessity. Professional interpreters aren’t optional. They’re essential. And patients who don’t speak English aren’t a burden-they’re people who deserve the same chance to be safe as anyone else.
The tools exist. The data proves it works. The cost of doing nothing is far higher than the cost of doing it right.
It’s time for every pharmacy to stop guessing-and start giving clear instructions in every language.


12 Comments
Teresa Marzo Lostalé-28 December 2025
Imagine being handed a pill bottle like it’s a puzzle you’re supposed to solve alone… and your life depends on getting it right. 😔 I’ve seen grandmas in my neighborhood nodding along like they understand, just to avoid looking ‘stupid.’ It’s not about language-it’s about dignity.
And yeah, Google Translate is a trap. My cousin thought ‘nebulizer’ was ‘nebula’-like space stuff. She almost drank it.
Why are we still treating health like a privilege for English speakers?
Mimi Bos-29 December 2025
so i just asked my local pharmacy for a spanish label and they said ‘we dont have that’ and handed me a printout with google translate on it. i was like… cool. thanks for the life sentence. 🤦♀️
Debra Cagwin-30 December 2025
As someone who’s trained pharmacy techs for over a decade, I can tell you this isn’t about cost-it’s about will. We’ve had bilingual label templates since 2019. We’ve had certified translators on contract for years. The problem? Staff don’t ask. Managers don’t enforce. Patients don’t know to demand it.
Let me be clear: if you’re not offering translation in the top 5 languages in your zip code, you’re not just cutting corners-you’re endangering lives. And if your system doesn’t auto-trigger translation when language preference is flagged? You’re still in the Stone Age.
It’s not hard. It’s not expensive. It’s just inconvenient for people who don’t have to live with the consequences.
ANA MARIE VALENZUELA- 1 January 2026
Oh please. You’re blaming pharmacies for America’s immigration problems? People who don’t speak English shouldn’t be on prescription meds without a family member who does. It’s not the pharmacy’s job to be a translator, a cultural advisor, AND a nurse. The system’s broken, sure-but you can’t fix it by making pharmacists into unpaid social workers.
And ‘professional translation’? At $5 per script? That’s $250K a year for a mid-sized pharmacy. Tell that to the owner who’s already losing money on Medicare reimbursements.
Stop pretending this is a moral failure. It’s a structural one. And no, your pretty visuals won’t fix that.
Bradly Draper- 3 January 2026
My aunt took her blood pressure pill wrong for months because the label said ‘take one at bedtime.’ She thought it meant right before she went to sleep, not that she should take it when she went to bed at night. She ended up in the hospital. No one asked her if she understood. No one even checked.
It’s not hard to say, ‘Let me explain this to you.’ But nobody does. And then they wonder why people keep ending up in the ER.
Gran Badshah- 4 January 2026
in india we dont have this problem because we dont give pills in english. we use hindi or regional language. why usa so lazy? also your doctors dont even know how to say ‘take after food’ in simple words. they say ‘with meals’ like its a fancy restaurant. smh.
sonam gupta- 4 January 2026
USA is weak. Other countries manage. Why cant you? You have money. You have tech. You have laws. But you still let people die because you dont want to print a second line. This is not a language problem. This is a moral failure. Shame on you.
Julius Hader- 4 January 2026
Look, I get it. But let’s be real-how many of these people even take their meds correctly even with perfect instructions? I’ve seen folks skip doses because they ‘felt fine.’ Translation won’t fix laziness or denial.
And let’s not forget: some people just don’t want to learn English. That’s their choice. But now we’re supposed to translate everything? What’s next? Sign language on every soda bottle?
Empathy is great. But responsibility matters too.
Vu L- 4 January 2026
‘62% reduction in errors’? Bro, that’s a cherry-picked stat from one study. I’ve worked in 3 different pharmacies. Most patients who don’t speak English just don’t take their meds anyway. The ones who do? They get help from family or use pill organizers.
Also, ‘universal symbols’? Ever seen someone try to interpret a sun icon? One guy thought it meant ‘take outside’ and took his pill on the porch in January.
This whole thing is performative activism. Real solution? Learn English. Or hire a translator. Not the pharmacy’s job.
Payton Daily- 5 January 2026
Let me drop some truth bombs. This isn’t about language. It’s about power. Who gets to be heard in a hospital? The ones who speak the right way. The ones who don’t? They’re invisible. And that’s by design.
Medicine has always been a gatekept system. The label isn’t just instructions-it’s a test. A test you fail if you don’t know the code. ‘Take as directed’? That’s not medical jargon. That’s a filter.
And don’t tell me about ‘visuals’-you think a red cross means ‘no alcohol’ to someone who’s never seen a hospital? You’re projecting your privilege onto their trauma.
Real change? Dismantle the system. Not translate the label.
Nicole Beasley- 6 January 2026
Just had to tell my mom to stop taking her insulin at night because the label said 'take at bedtime' and she thought bedtime = after dinner 😭 I cried. We had to call the pharmacy 3 times. They sent us a PDF. No one spoke Vietnamese. I had to translate it myself. Why does this still happen in 2025? 🥺💊
Julius Hader- 7 January 2026
Actually, I work with a pharmacy that just rolled out automated translation via their EHR. It’s not perfect, but it’s way better than before. We print bilingual labels now, and we have a tablet with video interpreters on standby. Patients are actually smiling now.
It’s not magic. It’s just… done right. And yeah, it cost money. But our error rates dropped 50%. Staff morale went up. Patients come back. That’s not activism-that’s business.
Stop acting like this is a charity. It’s smart medicine.