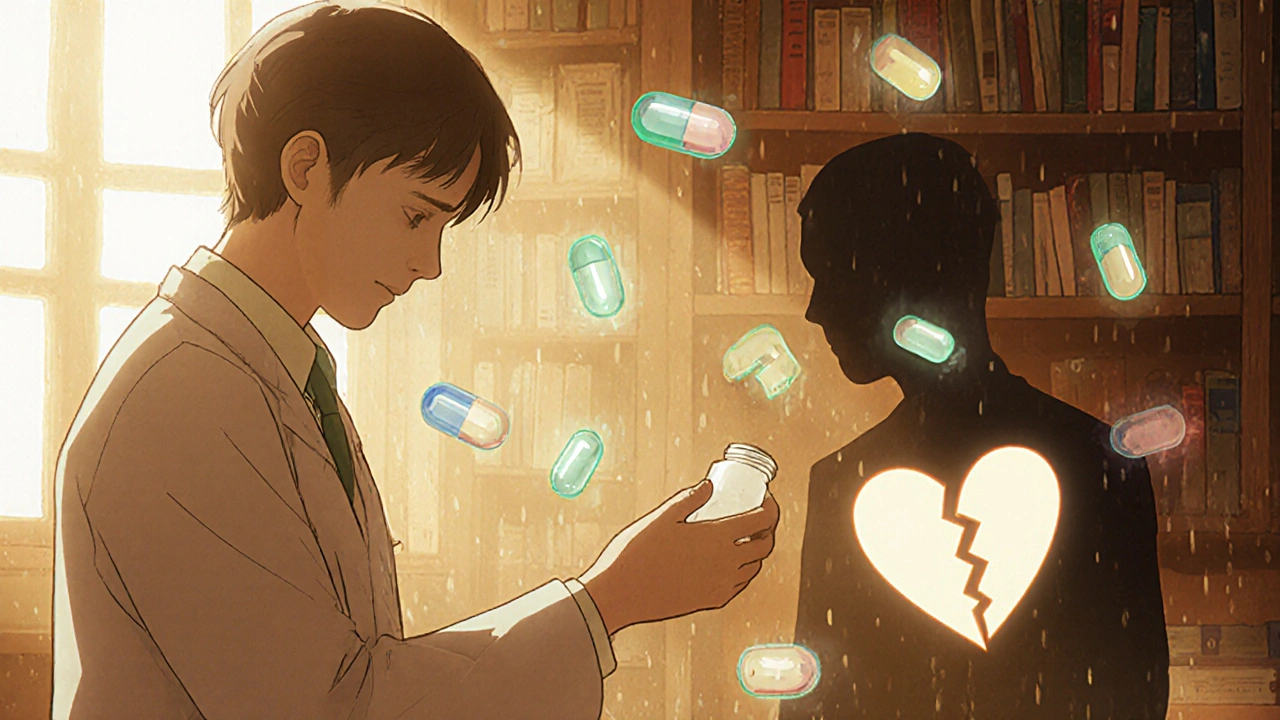
Switching from a brand-name drug to a generic version seems like a simple cost-saving move. But for some people, that switch triggers headaches, anxiety, seizures, or worse. If you’ve noticed a change in how you feel after your pharmacist handed you a different-looking pill, you’re not imagining it. And you’re not alone.
Why Switching Generics Can Cause Problems
Generic drugs are required to have the same active ingredient as the brand-name version. That part is true. But what’s not always said is that generics can differ in their inactive ingredients-fillers, dyes, coatings, and how the drug is released in your body. For most people, these differences don’t matter. But for others, especially those taking medications with a narrow therapeutic index, even tiny changes can be dangerous.Narrow therapeutic index means the difference between a safe dose and a harmful one is very small. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid issues), tacrolimus (for organ transplants), and certain seizure medications fall into this category. If your blood levels of the drug dip just a little too low, the treatment fails. If they spike too high, you risk toxicity. And switching between generic versions-even ones approved by the FDA-can cause those shifts.
A 2019 study in BMJ Open tracked over 2,800 people with heart disease who switched between different generic versions of the same drug. Within 30 days, they had a 12.3% higher chance of being hospitalized compared to those who stayed on the same formulation. That’s not a fluke. It’s a pattern.
Which Medications Are Most Likely to Cause Issues
Not all generics are created equal. Some drug classes have a much higher risk of problems after switching:- Antiepileptics (like divalproex sodium or phenytoin): A 2021 survey of 147 neurologists found that nearly 70% believed switching generics increased seizure risk. Some patients reported breakthrough seizures within days of a new refill.
- Thyroid meds (levothyroxine): With 12 different generic manufacturers in the U.S., even small changes in absorption can throw your hormone levels off. Symptoms? Fatigue, weight gain, brain fog, or heart palpitations.
- Anticoagulants (warfarin): Even a 10% change in how the drug is absorbed can increase your risk of clots or bleeding. Many patients need more frequent blood tests after switching.
- Immunosuppressants (tacrolimus, cyclosporine): For transplant patients, a switch can lead to organ rejection. One study showed a 27% increase in treatment discontinuation after inappropriate switches.
- Extended-release psychiatric drugs (like Adderall XR, bupropion XL): Different manufacturers use different bead-release systems. One generic might release the drug over 12 hours. Another might release it too fast, causing anxiety or insomnia-or too slow, causing symptoms to return.
These aren’t rare edge cases. They’re documented, repeatable problems. The FDA says generics are equivalent. But doctors and patients on the ground see something different.
What Real Patients Are Saying
On Reddit’s r/ADHD community, a thread titled “Generic Adderall Switch Ruined My Life” has over 800 comments. Most describe the same story: they were stable on one generic version. Then, their pharmacy switched them without warning. Within 24 to 72 hours, their focus vanished. Anxiety spiked. Sleep disappeared. Some even had panic attacks they’d never had before.A 2023 analysis of patient records at a major hospital found that 63% of people taking generic ADHD meds noticed reduced effectiveness after a manufacturer change. Over 40% reported new side effects-headaches, nausea, irritability. One patient developed serotonin syndrome after accidentally taking two different generics at the same time because she didn’t realize they were different pills.
It’s not just ADHD. People on generic antidepressants, anticonvulsants, and blood pressure meds report similar patterns. They don’t know why they feel worse. They assume it’s stress, aging, or their condition getting worse. But the timing lines up perfectly with their last refill.
Why This Keeps Happening
The real culprit isn’t the generics themselves. It’s the system behind them.Pharmacy benefit managers-companies like CVS Caremark and Express Scripts-control which generics pharmacies stock. They don’t care which manufacturer makes the drug. They care about rebates. The company that offers the biggest discount gets chosen. And they change that choice often. On average, PBMs switch preferred generic manufacturers 4.7 times a year per drug.
That means you could be on one version of generic levothyroxine in January. By March, your pharmacy switches you to another. Then again in June. And again in October. Each switch carries risk. And you might not even know it happened.
Some pharmacies don’t tell you. The pill looks different-maybe a different color or shape-but the label just says “levothyroxine.” You assume it’s the same. It’s not.
What You Can Do
You don’t have to accept this as normal. Here’s what actually works:- Ask for the manufacturer name when you pick up your prescription. Say: “Can you tell me which company makes this generic?” If they say no, ask to speak to the pharmacist. Most can look it up using the NDC code on the bottle.
- Write it down. Keep a small notebook or phone note with the name of the manufacturer and the pill’s appearance (color, shape, imprint). If you notice side effects, you’ll know if it’s a new version.
- Request “Dispense as Written” on your prescription. This tells the pharmacist not to substitute. You can ask your doctor to write “DAW-1” on the script. This is especially important for thyroid meds, blood thinners, and seizure drugs.
- Watch for changes in the first 72 hours. If you feel worse-more anxious, more tired, more shaky, or your symptoms return-call your doctor. Don’t wait. It could be the switch.
- Don’t assume all generics are the same. Even if two pills have the same name, they might come from different factories with different release systems. That matters.
A 2021 study found that patients who got counseling from a pharmacist about switching risks were 37% less likely to have bad outcomes. Knowledge is power.
When to Worry
You should be concerned if you notice any of these after switching:- New or worsening anxiety, panic attacks, or insomnia
- Return of symptoms you had under control (seizures, depression, high blood pressure)
- Unexplained fatigue, dizziness, or heart palpitations
- Headaches, nausea, or stomach pain that started right after the new refill
- Feeling “off” for no clear reason, but only after a pill change
If you’ve had one of these reactions, don’t brush it off. Go back to your doctor. Bring your pill bottle. Say: “I switched generics, and this happened.” Most doctors will listen. If they don’t, ask for a referral to a pharmacist who specializes in medication therapy management.
The Bigger Picture
The system is built to save money. And it does-generics save the U.S. healthcare system over $165 billion a year. But the hidden cost? Hospitalizations, ER visits, lost workdays, and people living in fear that their next refill might make them sick.Some progress is being made. In 2023, Medicare started limiting generic switches to no more than twice a year for its patients. Researchers are developing better tests for complex generics. But until the system changes, the burden falls on you.
You have the right to know what’s in your pill. You have the right to ask for consistency. And you have the right to speak up when something feels wrong. Your health isn’t a cost center. It’s your life.
Are all generic drugs safe to switch between?
For most medications, yes. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, tacrolimus, and certain seizure or ADHD meds-even small differences in formulation can cause serious problems. Always check the manufacturer and monitor for side effects after a switch.
Can I ask my pharmacist not to switch my generic?
Yes. You can ask for the same manufacturer every time. You can also ask your doctor to write "Dispense as Written" or "DAW-1" on your prescription. This legally prevents substitution unless you or your doctor approves it.
Why do pharmacies switch generics so often?
Pharmacy benefit managers (PBMs) get rebates from drug manufacturers. The company offering the highest rebate gets chosen. PBMs switch manufacturers up to five times a year to maximize profits-not to improve your care. This creates instability in your medication supply.
What should I do if I feel worse after switching generics?
Don’t wait. Contact your doctor immediately. Bring your pill bottle and note the manufacturer name. Track when symptoms started. Many doctors will switch you back or prescribe a brand-name version if necessary. Your health comes before cost savings.
Is there a list of generics that shouldn’t be switched?
Yes. The American Society of Health-System Pharmacists published a list in January 2024 that includes 17 high-risk generic drugs, such as bupropion XL, tacrolimus, phenytoin, and levothyroxine. These should be avoided for automatic substitution. Ask your pharmacist for this list or request a copy from your doctor.
Next Steps
If you’re on a high-risk medication, start today: check your last refill. Write down the manufacturer. Set a reminder to check your next one. Talk to your doctor. Ask for DAW-1. Keep a log. You’re not being difficult-you’re being smart.Generic drugs save money. But they shouldn’t cost you your health. If your body reacts, listen to it. You know your body better than any algorithm or rebate system ever will.




8 Comments
Elaina Cronin-21 November 2025
It is utterly unacceptable that pharmaceutical profit margins are being prioritized over patient safety. The FDA's equivalence standards are archaic, and the fact that pharmacy benefit managers are permitted to switch formulations without consent constitutes a systemic failure of medical ethics. I have personally witnessed a patient suffer a seizure after an unsanctioned generic switch-this is not anecdotal; it is criminal negligence.
Willie Doherty-22 November 2025
The BMJ Open study cited has a significant confounding variable: adherence. Patients who experience frequent generic switches are also more likely to be non-adherent due to confusion, which independently increases hospitalization risk. The data does not isolate pharmacokinetic variability as the primary driver-it conflates behavioral and biological factors. A multivariate regression analysis is required before drawing causal conclusions.
Darragh McNulty-22 November 2025
Thank you for writing this!! 🙏 I was on generic Adderall and started having panic attacks out of nowhere-thought I was losing my mind. Then I checked the bottle and saw a different manufacturer. Switched back to the old one and boom-calm again. 🎯 Don't let anyone tell you it's 'all in your head.' Your body knows. Keep track, speak up, and don't let them gaslight you. You're not crazy-you're just being ignored. 💪
David Cusack-22 November 2025
One must question the epistemological foundation of the assertion that 'inactive ingredients' are inconsequential-particularly when the pharmacodynamics of extended-release formulations are governed by polymer matrices whose bioavailability profiles are neither standardized nor transparently disclosed. The FDA's bioequivalence thresholds-80-125% AUC-are statistically permissive, not clinically protective. One wonders whether the regulatory apparatus has been captured by industrial interests. The data speaks; the public remains silent.
Debanjan Banerjee-24 November 2025
As a clinical pharmacist in India, I've seen this exact issue with antiepileptics and thyroid meds. In resource-limited settings, patients are often switched without documentation or counseling. The 2024 ASHP list is critical-every prescriber should have it posted. I now print the manufacturer name and NDC on every script for high-risk drugs. It takes 10 seconds, but it saves lives. Also, if your pharmacy won't tell you the maker, find a new one. This isn't paranoia-it's standard of care.
Steve Harris-25 November 2025
I’ve been a doctor for 22 years. I used to think generics were interchangeable. Then I had a transplant patient reject her kidney because her tacrolimus was switched twice in six months. I now write DAW-1 on everything for narrow-therapeutic-index drugs. I also tell patients: ‘If you feel different after a refill, call me before the weekend.’ It’s not expensive. It’s not inconvenient. It’s just the right thing to do. Let’s stop pretending cost savings are worth risking lives.
Michael Marrale-26 November 2025
Wait-so PBMs are switching your meds to make money? And the FDA is letting them? And no one’s talking about the fact that some of these generics are made in China and India with unregulated fillers? I’ve seen reports of heavy metals in levothyroxine. They’re testing for active ingredients, not contaminants. What if this isn’t about bioequivalence at all… but about poison? Who’s really behind this? Why don’t the media cover this? 🤔
David vaughan-27 November 2025
I'm not a doctor, but I've been on levothyroxine for 12 years. I started keeping a notebook: date, manufacturer, pill color, how I felt. When I switched from Mylan to Teva, my TSH jumped from 1.8 to 7.3 in two weeks. I brought it to my endo. She was shocked. Now I have a signed note from my doctor to never substitute. I also call the pharmacy every time I refill. It's a pain... but worth it. You're not being difficult-you're being vigilant. And that's smart.