Kidney Disease: What It Is, How It Affects Your Body, and What You Can Do
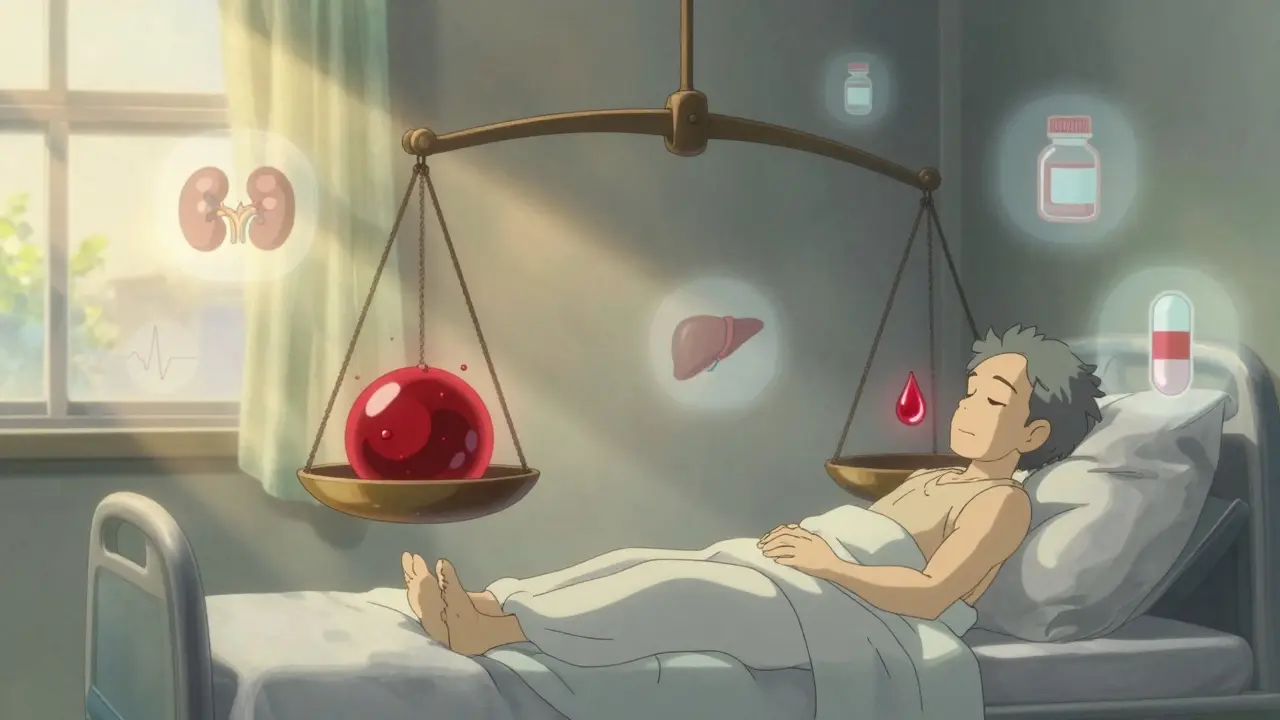
When your kidney disease, a condition where the kidneys lose their ability to filter waste and excess fluid from the blood. Also known as chronic kidney disease, it often creeps up without obvious symptoms until significant damage is done. Your kidneys don’t just make urine—they regulate blood pressure, balance electrolytes, produce red blood cells, and activate vitamin D. When they start failing, every system in your body feels the ripple effect. That’s why managing kidney disease isn’t just about drinking less water or cutting salt—it’s about understanding how it changes how your body handles every medication you take.
People with kidney disease, a condition where the kidneys lose their ability to filter waste and excess fluid from the blood. Also known as chronic kidney disease, it often creeps up without obvious symptoms until significant damage is done. often need to avoid common drugs like NSAIDs, certain antibiotics, or even some heartburn meds because their bodies can’t clear them safely. That’s why the medication safety, the practice of using drugs in a way that minimizes harm, especially when kidney function is reduced. Also known as renal drug dosing, it’s critical for anyone with reduced kidney function. becomes so important. A pill that’s harmless for someone with healthy kidneys can build up to toxic levels in someone with stage 3 or 4 kidney disease. Even common supplements or herbal products—like those marketed for liver or joint health—can stress your kidneys further. And if you’re on dialysis, your medication schedule changes entirely. Timing matters. Dosing changes. Interactions multiply.
It’s not just about pills, though. High blood pressure and diabetes are the two biggest causes of kidney disease, and both are deeply tied to what you eat, how active you are, and whether you’re monitoring your numbers. Many people don’t realize their kidneys are declining until they start feeling tired all the time, have swollen ankles, or notice changes in how often they urinate. By then, the damage is often advanced. But catching it early—through simple blood and urine tests—can slow or even stop progression. That’s why knowing the signs and understanding your lab results matters more than you think.
And if things get serious, dialysis, a medical treatment that filters waste and excess fluid from the blood when kidneys can no longer do it. Also known as renal replacement therapy, it’s a lifeline for many. becomes part of your routine. It’s not a cure, but it keeps you alive. Still, it brings its own challenges: strict fluid limits, dietary changes, and the risk of infections. Every medication you take after starting dialysis has to be re-evaluated. What worked before might not work now—and what you thought was safe might suddenly be dangerous.
This collection of articles doesn’t just talk about kidney disease in theory. It shows you how it connects to real-world medication risks—like what happens when you take a blood thinner with failing kidneys, why certain painkillers are off-limits, and how even something as simple as an OTC heartburn pill can become a hidden threat. You’ll find practical advice on spotting early signs, understanding lab results, and talking to your doctor about safe drug choices. Whether you’re managing kidney disease yourself, caring for someone who is, or just want to protect your kidneys before problems start, these posts give you the facts you need—no fluff, no jargon, just what works.
Anticoagulation in Kidney and Liver Disease: What Doctors Really Do
Managing blood thinners in kidney and liver disease is complex and risky. Learn what doctors actually do when guidelines don’t apply, which anticoagulants are safest, and how to navigate treatment when your organs aren’t working right.
Proteinuria: How to Detect Urine Protein and Stop Kidney Damage Early
Proteinuria means excess protein in urine - an early warning sign of kidney damage. Learn how to detect it, what causes it, and how to stop it before it leads to kidney failure.